John F. Mramor, MA, LMT, CLT, NCTMB, CR, RM
Medical Advisors:
Michael Harrington, MD, Director, Palliative Care Consult Service, MetroHealth Medical Center and Assistant Professor, Case Western Reserve University School of Medicine
Walter George, MD, Medical Director, Crossroads Hospice, Cleveland, Ohio
INTRODUCTION
Manual lymph drainage (MLD) is a gentle manual treatment technique developed by Dr. E. Vodder in France (Vodder, 1936). MLD is a main component of Complete Decongestive Therapy (CDT), which is a combination of:
1. MLD
2. Compression therapy
3. Decongestive exercises
4. Skin care
CDT is used to treat lymphedema/edema that is the result of neoplastic obstruction, postoperative interference with lymphatic flow, radiation damage to the lymphatic system, ascites or some congenital diseases (Badger, 2004). It is also employed in cases of reflex sympathetic dystrophy, rheumatoid arthritis, traumatic edema, lipedema, wounds and chronic venous insufficiency (Zuther, 2005).
Within hospice and palliative care settings, MLD is a great tool to maintain the patient’s quality of life. It is helpful in the management of the following conditions:
1. Lymphedema due to lymph node dissection, radiation scarring, tumor obstruction, ascites, deep vein thrombosis and associated with various diseases (Herpertz, 1990)
2. Recurrent cellulitis, especially for patients who are no longer able to ambulate or engage in exercise/independent ROM
3. Resolution of lymphatic fistulas (i.e., weeping skin)
4. Pain management, especially pain related to distension, compression or pressure by fluid
5. Wound healing, including formative and mild cases of gangrene and moderate to severe decubitis or venous ulcers
6. Negative self-image issues as a result of swellings;
7. Easing ambulation, transfers, positioning, dyspnea and care giving
8. Psychoemotional/social benefits and sleep normalization
Patients who have experienced MLD in a hospice setting noticed the psychological and spiritual transformations that occur as the hospice therapist companions them in their journey using the hand, mind and heart as a healing bridge. This is a profound difference from MLD delivered in a non-hospice setting.
MLD FOR ASCITES
The author stumbled on the application of MLD as a supportive therapy in the treatment of ascites quite by chance 10 years ago. Since the first successfully treated patient, MLD has proven useful in delaying the re-accumulation of ascitic fluid in cases of both malignant and cirrhotic ascites. The author has not conducted research to validate his clinical findings and experience thus far, but it is his hope that through the dissemination of this article, medical professionals and therapists will be inspired to pursue a study regarding this treatment option. In all cases MLD was prescribed by managing physicians and nurses and its application was under their control.
Employing MLD as a supportive therapy in the management of ascites delays the re-accumulation of fluid between abdominal taps (i.e., paracentesis), slows the accumulation of fluid in the initial, formative stages of ascites, reduces the amount of fluid drained through catheters or other devices, diminishing the chance of their failure. MLD does all of this by diverting the subcutaneous drainage of fluid from the inguinal lymph nodes into the axillary nodes.
To fully understand the mechanism of MLD let’s look into this subject closely. Normally, lymph drains through each segment of the body in two levels:
1. Superficial drainage through subcutaneous lymph channels
2. Deep drainage through lymph channels that support drainage from the viscera, bones, and muscles
Each part or segment of the body drains into a specific pack of lymph nodes. Neighboring areas which drain into different lymph nodes are separated by so-called watersheds. Fig. 1 illustrates lymphatic system with the location of main watersheds.
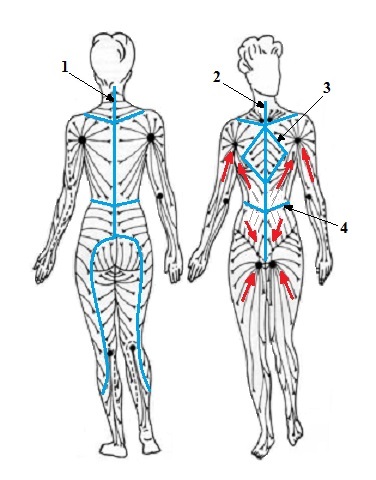
Fig. 1. Normal lymph drainage and watersheds (blue lines)
1 – posterior vertical watershed
2 – anterior vertical watershed
3 – thoracic watershed
4 – transverse watershed
Red arrows – direction of lymph drainage to axillary and inguinal lymph nodes
Please refer to Fig. 1. As you can see the upper parts of the abdomen (areas A and B) are drained into the axillary lymph nodes while the lower parts of the abdomen (areas C and D) are drained into the inguinal lymph nodes. These four areas are separated by watersheds (blue lines). Under normal circumstances lymph drains only within the area surrounded by watershed which prevents lymph to cross into a neighboring area and overwhelm drainage there. Thus watersheds are walls which surround the segment of the body which drains into the particular pack of lymph nodes.
In the case of ascites, fluid mostly is accumulated in the lower parts of the abdominal cavity since the force of gravity retains it there. MLD uses two pathways to assist drainage of fluid from the abdominal cavity. Fig. 2 illustrates how MLD diverts lymph flow and reduces ascites using Pathway 1.
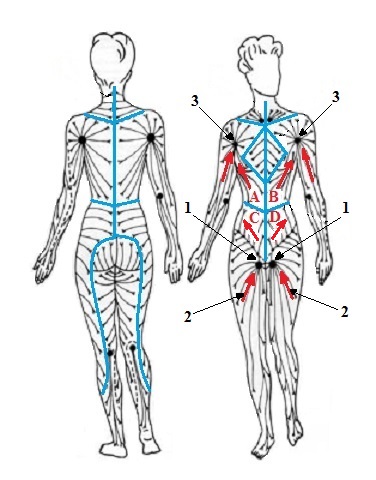
Fig. 2. Two pathways of MLD assist in drainage of ascitic fluid
1 – inguinal lymph nodes
2 – drainage from the lower extremities
3 – axillary lymph nodes
Pathway 1
The ascitic fluid is usually drained through the deep channels from the abdomino-pelvic region into the inguinal lymph nodes (Fig. 2, ‘1’). Additionally, all soft tissues in the areas C and D as well as lower extremities (Fig. 2, ‘2’)also drain their lymph into the same inguinal lymph nodes. As a result these lymph nodes become overwhelmed, exhausted, dilated, blocked or simply cease to function over time.
MLD diverts the lymph flow from the soft tissues of the abdomino-pelvic area from the inguinal lymph nodes into the axillary lymph nodes (Fig. 3, ‘3’). Increased interstitial pressure during MLD allows fluid from soft tissues in area D be pushed over the watershed into the area B and later into axillary lymph nodes. The same will happen with drainage enhanced by MLD between areas C and A. It greatly unloads packs of inguinal lymph nodes and reduces ascites.
This diversion is made possible due to the existence of a subcutaneous lymphatic anastomoses between two neighboring areas separated by a common watershed. Through these anastamoses, the therapist can route a substantial amount of fluid from one area into the other. This not only improves subcutaneous lymph flow, but also creates a pressure gradient which drains some fluid from the abdominal cavity into axillary lymph nodes through the connections that exist between both superficial and deep networks. Additionally MLD increase the lymph drainage through the lymphatic plexus, spider web-like formation of lymphatic vessels which additionally helps to drain fluid between both networks.
Pathway 2
Fluid in the abdominal cavity tries to use any possible means to drain itself. While MLD diverts lymph flow from the lower abdominal areas into the axillary lymph nodes it creates a ‘vacuum’ effect which helps ascitic fluid to drain from the abdominal cavity into the soft tissues of the abdomino-pelvic region first (areas C and D in Fig. 2) and from there MLD can drained it further into the axillary nodes using Pathway 1.
MLD benefits the patient with ascites in numerous ways:
1. A decreased number of trips to hospitals for punctures. It saves energy necessary for travel, and the discomfort of the procedure itself and diminishes the patient’s financial burden
2. Longer periods of comfort between abdominal taps
3. Prolonged decrease in pain related to abdominopelvic distension pressure, diaphragmatic compression against the sternum and lungs, and compression of the viscera
4. Decreases edema in the lower and upper extremities
5. Improved self image
6. Longer periods of respiratory ease
7. Decreases pressure on working catheters or other devices
8. The enormous psychological benefit of touch which is especially important to patients who face the end of life
Generally, all patients are candidates for MLD, especially once they are admitted into a hospice or palliative care program. According to the medical advisor, there are no contraindications to preclude the use of MLD in ascites (Harrington, 2011 and 2012). No patient should be denied touch; it is the job of the therapist to find a safe and effective manner in which to deliver it. However, from the perspective of the author, there are contraindications that must be discussed.
ABSOLUTE CONTRAINDICATIONS
Spontaneous Bacterial Peritonitis (SBP)
Acute Deep Vein Thrombosis
Acute Cellulitis
Shingles
Infectious skin diseases
Mottling and other signs of approaching death
Hallucinatory/delusional behaviors
Systemic generalized edema
Severe systemic infections
Cancer or metastasis within the lymphatic region to be worked with
As the treatment progresses, there are many indicators signaling MLD success:
1. The time interval between abdominal taps increases and a lesser amount of fluid is drained
2. The depth of respiration improves
3. Fewer gastrointestinal complaints
4. Tolerance of physical activity increases
5. Weight decrease
- 6. A measurable decrease of peripheral edema
The following short case study illustrates the effectiveness of MLD. It involves the very first patient to be treated by the author.
CASE STUDY: LAUREN
Lauren was an eighty year old female who suffered from advanced stage breast cancer with lung and liver metastasis. Secondary diagnoses included diabetes and congestive heart failure. Accompanying medical concerns were: left mastectomy with removal of 17 nodes; lymphedema of the left arm and edema of the lower extremities; and most significantly, ascites requiring paracentesis every 15 days with four to five liters typically drained with each puncture. Her weight fluctuated from a baseline of 125 lbs. to 140-150 lbs. as the ascites worsened.
She was placed in a residential hospice from her home just prior to therapy. The referral was made by the hospice RN, who suggested MLD to the left arm due to swelling, discomfort and decreased mobility. However, after the patient’s evaluation a decision was made to use MLD to assist with the ascites management instead, lessening the need for paracentesis. This seemed to be of greater value due to the side effects of ascites: orthopnea, abdominal organs compression, diaphragmatic compression, shortness of breath, lymphatic fistulas, cellulitis of the left leg, ambulatory difficulties and poor self-image. The patient also slept only in an upright position in a rocking chair. Also it was obvious that the left arm could improve only after the fluid accumulated in the subcutaneous tissues of the chest wall and abdomen had been drained.
MLD was initiated immediately after an abdominal tap (i.e., paracentesis). A total of four liters were removed with her weight at 140 lbs. prior to puncture. Treatments were scheduled daily, 5 days a week, in the morning prior to breakfast. Both the RN and patient were quite surprised to witness a delayed need for a subsequent paracentesis. It was delayed an additional 14 days, thus making it a total of 29 days since her last puncture. When the paracentesis was performed, only three liters were removed with her weight prior to puncture at 133 lbs.! The patient survived another 2.5 months after this puncture, without need for another paracentesis and the whole while on a routine MLD schedule. Her legs and left arm also reduced in size.
In the Part III of this article we will present the MLD protocol for ascites.
REFERENCES
1. Badger C, Preston C, Seers K, Mortimer P. (2004) Physical therapies for reducing and controlling lymphoedema of the limbs. Cochrane Database of Systematic, 4:CD003141.
2. Harrington M. Director, Palliative Care Consult Service of MetroHealth Medical Center and Assistant Professor, CWRU School of Medicine. Personal communications. March 26, 2011 and March 20, 2012.
3. Herpertz U. (1990) Significance of radiogenic damage for lymphology. Z. Lymph, Dec;14(2):62-7
4. Vodder E. Le drainage lymphatic, une nouvelle methode therapeutique. Sant pour touts, 1936
5. Zuther J. (2005). Lymphedema management. New York, USA: Thieme Medical Publishers.
Category: Medical Massage
