Dr. Ross Turchaninov, Phoenix, AZ
A month ago, a patient we helped with different somatic syndromes over the course of the past 10 years asked us for a second opinion before deciding on right shoulder surgery.
The patient is a 77 year-old woman who is relatively active and takes care of her partially disabled husband. More than 10 years ago she got chicken pox, which triggered severe Trigeminal and Minor Occipital Nerve Neuralgias.
The patient still feels residuals of that in the form of very frequent attacks of itching on the right side of her face and right temporal area. To reduce the itch intensity, she is forced to constantly touch, rub or compress her right temporal area and right face.
HISTORY OF PRESENT ILLNESS
The patient complained about acute pain every time she lifted her right arm forward and pain with abduction. She was seen by her PCP who sent her to an orthopedic surgeon.
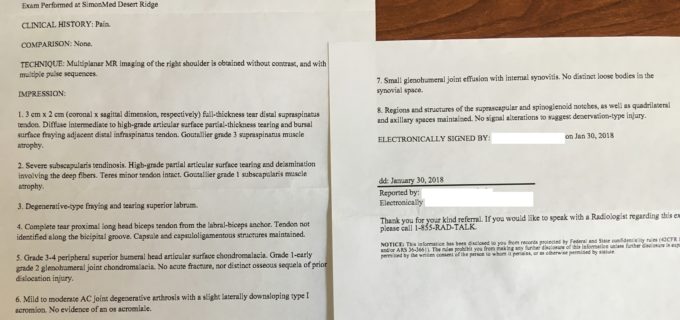
The surgeon ordered a right shoulder MRI which showed damage and deterioration in practically all major components of the shoulder joint: full thickness tear of supraspinatus tendon; partial tear of infraspinatus tendon; tear and severe tendinosis of the subscapularis muscle with its atrophy; tear of the superior labrum; complete tear of the tendon of the long head of the biceps from the bicipital groove; Grade 4 softening of the bone in superior part of the humeral head; synovitis and accumulation of fluid in the joint cavity. Fig. 1 illustrates the radiologist’s report.
Fig. 1. Radiologist’s report of our patient
The surgeon immediately suggested reconstructive surgery due to the profound changes in her shoulder joint. He also mentioned that the surgery would be extensive with up to 6 months of rehabilitation after. Considering her husband’s condition, the patient declined surgery at this point and the orthopedic surgeon suggested 15 sessions of PT and possible steroid injection in the shoulder, but he told the patient that considering the intensity of damage, there is no way she will be able to fully function without shoulder surgery.
The patient went to PT and by approximately the 10th session she stopped since the pain intensity dramatically increased. She came back to the surgeon and he did a steroid injection in the joint and it decreased pain intensity by approximately 20%. She said that injection brought her back to the level of pain she had before her first PT session. She made an appointment with the surgeon for presurgical consultation and decided to stop in our clinic for a second opinion.
EVALUATION
One part of the clinical interview was very puzzling. When we asked the patient how the pain in the shoulder started she mentioned that she noticed it 3-4 months ago as a little discomfort which eventually grew and became very acute. Finally, she started to avoid shoulder usage.
The patient didn’t have any trauma to the shoulder before the pain started. It was surprising since such profound changes in the shoulder must be accompanied by significant traumatic force. According to the patient she fell and traumatized her shoulder almost 20 years ago. So, these two facts didn’t match.
She didn’t feel significant discomfort at rest and she felt pain starting with every active movement. Also, the pain bothered her at night and she’d wake up every time she needed to roll on either side.
Evaluation indicated visual elevation of the right shoulder with a simultaneous slight tilt of her head to the right, restriction of active flexion (see Fig. 2a) and active abduction (close to 80 degrees). Passive abduction was also restricted to 80 degrees and inner rotation was very painful (these are signs of early stages of frozen shoulder). Palpation of the supra, infraspinatus, subscapularis, and biceps brachii is very painful with multiple locations of active TPs.
Further evaluation produced surprising results. While the patient was at rest in the sitting position and the Wartenburg’s Test for the Anterior Scalene Muscle (ASM) was applied, the patient felt acute pain in her right shoulder similar to what she usually experienced during active movements. Usually she was comfortable while sitting at rest.
TREATMENT
The patient had a final appointment with the surgeon in 10 days and we suggested that she let us work on her neck and shoulder during this time and see if application of MEDICAL MASSAGE PROTOCOLs would make any difference. From our perspective, evaluation indicated that her pain in the shoulder was at least partly triggered by tension in the ASM and it was referring a pain pattern from the axillary nerve’s irritation on the anterior neck. However, medicine is an unpredictable type of science and further confirmation can be obtained only after proper therapy is used. The patient agreed.
During her first two sessions we concentrated on application of MEDICAL MASSAGE PROTOCOL for ASM. We suggested her homework (hourly application of passive stretches, exercise in the water, changing pillow, etc).
The pateint felt 50% pain reduction even after the first session. During sessions 3 and 4 we added elements of MEDICAL MASSAGE PROTOCOL for Rotator Cuff Syndrome. Our forth session was on Wednesday, the day before the patient’s final meeting with the orthopedic surgeon on Thursday. By Thursday morning she didn’t have any pain in her right shoulder with full ROM. Fig. 2 illustrates our patient’s ROM during her first session and at the end of fourth session.
Fig. 2. Active flexion before first session of Medical Massage (a) and after fourth (b) session.
The patient’s daughter accompanied her mom to the meeting with the orthopedic surgeon. After leaving his office they almost at the same time remarked to each other, “Don’t you think that doctor was visually upset with such shoulder improvement and wasn’t able to hide it?”
It is more than a month now since our last session and as we agreed with the patient, she had a control visit in our clinic yesterday. She didn’t have pain in the shoulder and has full ROM. She does her supportive homework faithfully on a daily basis.
LESSONS:
1. This case isn’t unique for our clinic or clinics associated with SOMI. It stands out because of the intensity of damage within the shoulder joint. The initial trauma of the shoulder was many years ago, but pain the patient felt was coming from the chronic irritation of the brachial plexus by the ASM muscle on the anterior neck which mimicked pain in the shoulder itself. This is why her symptoms were slowly creeping instead of acutely starting.
2. Let’s recreate the chain of clinical events in our patient’s case: very frequent elevation of the right shoulder with simultaneous tilt of the head to the right to combat itching on the temporal area and right face —-> tension in the ASM which chronically irritated part of the brachial plexus which gave origin to the axillary nerve on the anterior neck —-> condition of hyperirritability of nociceptors in the deltoid muscle and activation of pain analyzing system —-> acute spasm in the deltoid muscle —-> elevation of pressure within the shoulder joint which pressed the head of the humerus against the scapula —-> increased pressure generated heat during repetitive movements and extra synovial fluid is accumulated inside of the joint —-> synovitis of the shoulder —-> softening of the bone —-> restricted ROM —-> early stages of frozen shoulder.
3. We guarantee readers that a majority of somatic syndromes therapists are working with a hidden neurological trigger which needs to be identified and removed first, before local therapy including various kinesiology-based therapies is applied. Only the presence of previous trauma, which the patient always remembers, justifies initial application of local therapy.
4. Correct evaluation of the local changes in the skin, fascia, skeletal muscles and periosteum on a layer by layer basis and the mandatory evaluation of the pattern of innervation of the affected area with identification of a hidden neurological trigger the is foundation for quick and stable somatic rehabilitation. Thus, relying on the local symptoms, the patient’s presents become an endless chase of one’s tail.
Category: Blog