In the Mar/Apr, May/June, July/Aug and Sept/Oct 2009 issues of JMS, we published a four-part article on Trigger Point Therapy (TPT). Since then we have read several articles on this subject, and participated and observed many discussions in professional forums on the same subject. This personal experience convinced us to return to the issue of trigger points and TPT one more time in the form of a follow-up article.
While working on the original article, we were sure that the science of TPT was well-known and an already settled issue. We saw the purpose of our original article was to put main theoretical and clinical components under the one roof. To our big surprise, participating in professional forums and reading recent articles reveled that TPT remains a most controversial, misunderstood and misrepresented issue.
We also realized that our attempts to express scientifically and clinically based opinions in the majority of cases were seen as just our personal opinion/theory. This is why we decided to address one more time the TPT issue from a scientific point of view and update the original article.
First, we would like to summarize the most common misunderstandings and simple mistakes the issue of TPT generated.
1. Trigger point is a local pathology without any involvement of the nervous system.
2. There is no scientific data which supports the theory that trigger points can be results of any neurological abnormalities or reflex zones formation.
3. The best way to eliminate the trigger point is through application of mild to moderate pressure.
4. The ischemic compression as a part of TPT is useless because it is not logical to treat the trigger point where circulation is already compromised by additional oxygen deprivation of the affected tissue.
Some of these ideas started to circulate in the massage community after publication by Dr. J. Muscolino (2008) on this subject. We greatly respect this author. He is in the minority of educators who really knows what he writes and teaches. However, we completely disagree with his views on the subject of TPT.
Recently, the situation became even more complicated when other practitioners and educators contributed to the confusion with their own ideas rather than scientifically based information. Frequently, statements are made without any data or references and as soon as authors are confronted on the origin of their ideas we heard similar replies: “I practice TPT for 20 years”, “I wrote books on TPT”, “I have taught TPT for 15 years”, “200 MD’s were impressed with my treatment” and so on. In other words “I can’t be wrong because I am right.”
We think that at this point the American massage therapy industry lacks unified view on majority of important subjects. A great number of educators espouse their own ideas and agendas without even bothering to examine scientific data that already exists but in many cases undermine their personally developed concepts and system of believes. Some educators mislead readers by manipulating existed data (Good/Bad Apples in the Nov/Dec 2010 issue ofJMS).The sad part is that many educators do not even agree with each other and teach completely opposite approaches, which dramatically increases the confusion. AMTA is just an observer of this contradictory state without the means and desire for the leadership.
As a result of all these events, the massage therapy practitioner trying to break into the medical field frequently relies on personal opinions, anecdotal experiences rather than on firm scientific data. We agree with the fact that every practitioner is entitled to their own opinion. However, this freedom stops at the moment the practitioner starts to work on the patients rather than clients. At this moment, the personal views become invalid if they are not supported by scientific data. This is why we decided to revisit the issue of TPT as one of the most misrepresented one. Although, this article is long, we encourage the reader to finish it because we believe our views will benefit everyone in the profession.
Trigger point is a local pathology without any involvement of the nervous system
There is a belief that trigger point is a local pathology without any involvement of the nervous system. This belief system absolutely correctly describes the chain of events that are responsible for the formation of a trigger point: Excessive calcium release, formation of taut band, shortage of ATP, local ischemia and so on. However, supporters of this view fail to provide any reasonable explanation for what actually triggers these events.
Yes, it is correct that a trigger point could be the result of trauma and this is one of the possible causes. Yes, the trigger point could form in the muscles that are overused especially if they are worked a lot in the isometric regime. For example, trigger points in the trapezius muscle of the computer programmer. In these two cases, the trigger points are indeed a local pathology as a result of direct trauma or chronic overload and they developed secondary to overused muscles.
However, this theory fails to explain commonly observed clinical facts of active trigger points formation in the muscles innervated by irritated or compressed spinal or peripheral nerve. Why, for example, the patient with acute disk bulging or herniation almost immediately exhibits active trigger points in the piriformis muscle or in the peroneal group? Any practitioner who works on patients with irritated or compressed brachial plexus finds trigger points in various locations on the upper extremity, and the location of these trigger points will coincides with the irritated part of brachial plexus. We can continue and continue with these examples.
The readers may ask: Is there any merit in this discussion? What is the difference if the nervous system plays or does not play a role in the formation of trigger point? The answer to what looks like these purely theoretical questions is very simple: Success of your entire practice is in stake!
Those who read various professional forums may regularly see pleas from the practitioners for help who desperately trying to eliminate ‘stubborn’ trigger point without any success. Why is that? The answer is very simple: Those practitioners approached active trigger point as a local pathology exactly what proponents of this theory recommend, instead of finding the real cause of the problem. In this case mild irritation of the nerve that supplies muscle harboring active trigger points. The practitioner is knocking on the same but unfortunately wrong door and this is reason for the failure. Trigger points are the result of many different factors, and the treatment protocol should consider and address the original cause otherwise the practitioner shouldn’t expect quick and sustained results.
Considering that the majority of authors use their personal experience or beliefs as a justification for this and similar concepts, we decided to present our personal experience as well. We conducted very basic research that examined the results from two clinics, one in Phoenix, Ariz., and another in Los Angeles. Calif. Evaluation of the our patients’ initial clinical symptoms and outcomes of the therapy for the month of August 2011 allowed us to conclude that 86% of our patients (320 total treatments) had somatic abnormalities accompanied by active trigger points in the skeletal muscles. From this 86%, approximately 70% were cases when active trigger points were a complication of the spinal or peripheral nerve entrapment. Our treatment protocols initially targeted the area of irritation and later local therapy in the area of active trigger point was added. We aren’t pretending on statistical proof of this data. This is our personal clinical observation.
Conclusion: the active trigger points are results of local abnormalities as well as involvement of the nervous system. We personally think that in the clinical practice the majority of the patients who have active trigger points have nervous system involvement, including viscero-somatic reflexes in cases of inner organ disorders, and to successfully eliminate these pathology local treatment isn’t enough. It is recipe for failure.
There is no scientific data which supports theory that trigger points can be results of any neurological abnormalities or reflex zones formation
This is the most bizarre statement we ever read. Even from historical point of view the proponents of this statement are wrong. They originated the concept of trigger points solely to the works of J. Travel MD. It is great misunderstanding to see Dr. Travel as the author of the trigger point concept. A great numbers of scientists have contributed to the development of trigger point concept way before Dr. Travel was even born:
Dr. R. Froriep (1843) was first scientist who studied trigger points;
Dr. H. Nothnagel (1877) proposed the original theory of the neurological origin of trigger points in the skeletal muscles;
Dr. H. Schade (1921) developed the concept of myogelosis as the outcome of chronic presence of trigger point;
Dr. J. Mackenzie (1923) proved that changes in the motor activity of the patient’s nervous system are key components in the development of hypertonic muscular abnormalities, especially trigger points. Thus, Dr. Mackenzie was the first to formulate the concept of reflex zones in the skeletal muscles, including trigger points.
As you can see trigger points were intensely studied since the end of 19th century and these scientific studies greatly influenced Dr. Travel’s and Dr. Simons’s work.
Supporters of local theory of trigger point formation widely cited selective quotes from Dr. Simmons’ earlier articles. It seems they use outdated data to reinforce their concept while Dr. Simons moved with the times and concluded that the nervous system is a major factor in the formation of trigger points. He endorsed the works of German scientist Dr. S. Mense and even co-authored an article on this subject (Hoheisel et al., 1993).
According to this experimental study, the triggering muscle pain leads to projection of these signals within the dorsal horns of the spinal cord, which in turn trigger referred pain and formation trigger points in completely new areas. Thus, the nervous system is directly responsible for the trigger point formation in the skeletal muscles or in other words in the areas of reflex zones.
Recently, some authors have started to return to the original theory that active trigger points are mostly the result of nervous system abnormalities. This theory was originally proposed by Dr. Nothnagel in 1877 and later was replaced by Travel’s and Simons’ works, which concentrated on the explanation of the local events within trigger point.
We are sure that it will surprise supporters of the strictly local theory of trigger points formation that overall frustration the unsuccessful treatment of trigger points has forced some scientists to abandon completely the local theory in favor of the original neurological theory (Quintner and Cohen, 1994). We are sure that such an opposite extreme is an equally incorrect view as the local theory, and both mechanisms are equally responsible for the trigger point formation. In many cases both mechanisms even contribute to the clinical picture in the same patient.
Another example of why supporters of the local theory are wrong is the fact that active trigger points are formed in the skeletal muscles as a result of various visceral abnormalities. This is one of the greatest contributions of Dr. Travel to medicine. She and Dr. Simons later showed without any doubt that active trigger points form in the skeletal muscles (e.g., pectoralis major and minor, trapezius, etc) of patients with chronic and acute cardiac disorders. As the original works of Dr. Travel showed, the deactivation of active trigger points in the chest and upper shoulder muscles significantly decreased the intensity of the chest pain even in patients with acute myocardial infarction (i.e., heart attack) (Rinzler et al., 1954). Additionally, active trigger points in the skeletal muscles do not easily disappear even after cardiac circulation is restored and the patient survives the heart attack (Landmann 1949).
Considering that formation of active trigger points in cases of visceral abnormalities is an undisputed established medical fact, the local origin of trigger point alone simply does not make common sense. For the active trigger points to form in the pectoralis muscles immediately during a heart attack, the nervous system must be involved. This is a perfect example of reflex zones formation and the supporters of the local theory usually do not mention this fact because it undermines the entire ‘local only cause’ concept.
Conclusion: claims that there is no scientific data that support the nervous system as one of the leading causes of trigger point formation means only one thing. The supporters of the ‘local only cause’ concept do not know or do not want to acknowledge the entire scientific data that completely rejects local only origin of trigger points formation. We can’t even believe that we are discussing this issue in the 21st century!
Even our short review of articles shows how wrong proponents of the local theory are and how confusing this subject for the practitioners who waste their time on useless treatments trying to eliminate active trigger points with local only treatment approach. The scientific and clinical data show that trigger points cannot be addressed as local pathology only. Such views will complicate and derail medical massage treatment and prolong patient suffering.
We treat patients in our clinics who initially have received incorrect somatic rehabilitation based on the local treatments applied by chiropractors, physical therapists and massage practitioners and in many cases lack of clinical success forced patients to undergo unnecessary surgeries, which could be prevented if correct MEDICAL MASSAGE PROTOCOL was chosen.
The best way to eliminate the trigger point is application of mild to moderate pressure
The supporters of this idea can be split in two camps:
1. Those who advocate that sustained mild pressure must be used because active trigger points are result of psychological conflict and such gentle pressure is comforting factor which helps the clients to balance their emotional state and thus eliminate active trigger points.
2. Those who advocate that moderate repetitive pumping strokes must be used to mechanically enhance arterial blood supply and venous drainage.
Both groups oppose the application of ischemic compression: The first one on spiritual grounds while the second one is based its logic of the fact that an active trigger point is an area of ischemia and it does not make any sense to impose additional ischemia to already ischemic tissue. We will address the issue of ischemic compression below.
Ironically, both groups are correct in their own belief but their supporters failed to see bigger picture. The body is a very complicated but efficient machine, and it always will defy those who use a simplistic approach.
Yes, active trigger points always will be exaggerated by emotion stress and, in these cases, the mild pressure is a correct clinical tool to address the tissue as a first component of TPT. It helps the patient to adopt and be comfortable with the practitioner while accomplishing the very important goal of desensitizing the area of the active trigger point by using application of massage therapy in the inhibitory regime. It allows the elevation of the threshold of peripheral receptors especially pain receptors in the area of future TPT.
Yes, pumping strokes in the area of the active trigger point is an equally important tool. Such strokes in combination with following application of permanent fixed vibration help to trigger local vasodilation using mechanical force, which prepares the active trigger point to the application of ischemic compression. This is one of examples of why application of ischemic compression only, is not enough but integrative approach to the TPT is the only correct clinical solution.
However, both groups make the grave mistake by singling out each of these tools from the context of TPT and using them as independent therapies. Such a one-sided, simplistic approach to TPT confuses the practitioner, and is directly responsible for the unsuccessful cases of TPT so frequently reported in the posts in various forums.
Conclusion: The ultimate success of TPT lies in integrative combination of treatment tools and is the only way to eliminate active trigger points with stable clinical results.
The ischemic compression part of TPT is useless because it isn’t logical to treat a trigger point where circulation is already compromise with additional oxygen deprivation of the affected tissue
As we discussed above, the supporters of this concept based their ideas on what seems to be reasonable logic: The active trigger point is area of ischemia and it makes no sense to impose additional ischemia to the tissue with already compromised circulation.
To support this assumption, the Second Edition of Trigger Point Manual by Travel and Simons is cited:
“deep-stroking massage as being … probably the most effective way to inactivate central TrPs when using a direct manual approach.”
First of all this was the personal opinion of Dr. Simons. When this quote is read carefully, the word ‘probably’ does not reflect the firm belief and conviction even from Dr. Simons himself. The fact that this single quote is a personal belief is supported by the fact that Dr. Simons did not measure clinical outcomes of only deep stroking massage against the ischemic compression. Without such study which would confirm one way or another, such a quote remains a personal opinion and this is exactly why Dr. Simons uses the word ‘probably’.
Those who are familiar with his publications have witnessed many times that he was very forceful in expressing his opinions (usually in form of letters to editors of scientific journals) when he was sure of his views. Here is one of the examples: Simons (2007).
The Trigger Point Manual is definitely remarkable book. However, we would like anyone who has access to it or own this publication to open the book and look at the treatment options Manual offers. The readers will find that this book offers the following treatments: injection, muscle energy techniques, cold and stretch approach (in the first edition) and lifestyle modifications. Massage as a treatment option mentioned one time at the beginning of the Volume I in the general chapter where all possible treatment options are reviewed.
Thus, neither Travel nor Simons considered massage as a valuable clinical tool. Otherwise massage options including deep stroking will be offered to the reader as a treatment option in each chapter. So why is that? Both Volumes are written by the physicians for physicians and in a lesser degree to physical therapists. The massage practitioners were not the original target audience. Plus neither Travel nor Simons personally used or studied massage therapy as a main treatment tool for their patients.
Now we would like to take our readers, especially those who believe that ischemic compression is outdated and even harmful tool, on a short journey into the most scientifically trusted source of modern understanding of circulation in the skeletal muscles written by Dr. R.J. Korthuis: Skeletal Muscle Circulation (2011).
Let’s look in Fig. 1 from this great book,which we highly recommend to those interested in this subject.
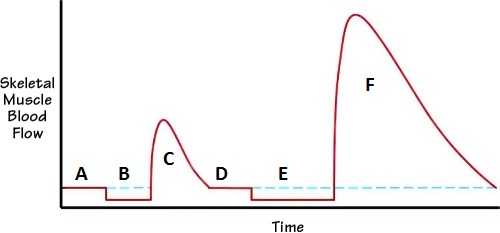
Let’s read this diagram.
A – baseline of circulation in the skeletal muscles before occlusion
B – occlusion of circulation less than 1 minute
C – reflex vasodilation after occlusion
D – restoration of the circulation to the baseline
E – occlusion of circulation more than 1 minute
F – reflex vasodilation after occlusion
Please pay attention to the difference in peaks of reflex vasodilation (C and F) in regard to their intensity (height of the vasodilatory wave) and duration (time of the vasodilatory wave) after occlusion less than 1 minute (B) and more than 1 minute (E).
Here is quote from the book (Korthuis, 2011) which illustrates Fig. 1.
“When the arterial inflow to skeletal muscle is suddenly occluded, blood flow decreases (B). Upon removal of the occlusion, skeletal muscle blood flow is markedly enhanced (C). The magnitude of this reactive hyperemia, both in terms of peak response and time to recover to baseline (D), varies directly with the time of occlusion. When the occlusion period exceeds 1 minute (E), maximal peak responses are achieved (F), but the time for blood flow to return to control levels is progressively increased.”
If anyone still has doubts, here is the final scientific medical data, but we are not done yet. We think it is extremely important to our profession to finally put this issue to rest. We recognize that it does not matter how many references we will use to support scientific foundation of TPT, this article will have limited influence on the followers of deep-stroking concept. Some of them exhibited very strong convictions. This is why instead of going back and forth with references, we decided to use visual proof of effectiveness of ischemic compression and illustrate it with a couple of very informative tests. This discussion became so complicated by conflicting opinions that we think that it is better to actually see how everything works rather than read conflicting opinions.
TEST 1. Reflex Vasodilation in the Normal Tissue
As we discussed above, the supporters of the only deep stroking massage treatment deny the fact of reflex vasodilation is a result of ischemic compression. Using simple application of Test 1, we can visually prove the existence of such phenomenon in the normal unaffected tissue. It is sad that this basic physiological mechanism requires extended discussion and prove for the practitioner who confused by inaccurately presented information.
Please pinch the skin on your inner forearm for one minute. The pressure should be significant but just below the pain threshold. In such a case you are creating ischemic compression in the skin on the forearm. After you release compression, the immediate picture you will see is a white spot that matches the compressed area. This is local ischemia as a result of skin compression. Soon you will see that this white spot changes color to pink or red. This is reflex hyperemia or direct evidence of vasodilation as a result of ischemic compression. However, this vasodilation is not the result of mechanical effect of effleurage/friction strokes (you just compressed skin). This vasodilation is a direct result of oxygen deprivation in the compressed tissue. In other words, cutting blood supply to the compressed tissue triggers reflex vasodilation, because the body will do anything to restore oxygenation of the tissue that has experienced even a short period of hypoxia.
To do that the reserve capillaries must be open, and this allows an extra amount of oxygenated blood to rush into the compressed tissue that you observe as skin redness. In a minute the skin color restores and it means that reserve capillaries are now closed and normal circulation is restored. This exact chain of events happened in the area of the active trigger point in the skeletal muscle and this is why ischemic compression is an important tool which, of course, should be combined with proper preparation of the soft tissues in the form of effleurage and deep pumping strokes. Thus, by finishing this simple experiment you prove to yourself that temporary applied local hypoxia from ischemic compression triggers local vasodilation using reflex mechanisms (e.g., axon reflex; see Vasodilation article in this issue of JMS).
Test 2. Dermographism Test (DT)
Our opponents may have a reasonable counterargument that Test 1 does not prove anything because it was used on the tissue (skin in our test) that initially had normal circulation and the trigger point is area of local ischemia where there is insufficient local circulation. Such final doubts can be easily put at rest by using more sophisticated Dermographism Test that we would like to discuss here as well.
DT is a much more complicated test and diagnostic tool. To fully understand value of DT we need to discuss first what dermographism means and how it looks in healthy person (see Video 1).
DT on the inner forearm of the healthy person
The best way to trigger DT is to quickly strike the skin with your fingernail (see video above). In the video above you see that immediately after we stroked the skin the white line appeared along stimulated part. This line is called white dermographism and it is the result of reflex vasoconstriction as a response to skin stimulation. Almost immediately quickly this line started to turn pink and later red and this new reaction to the initial skin stimulation is called red dermographism. The red dermographism is reflex vasodilation, which normally appears after initial vasoconstriction. The red line slowly fades away and original color of the skin in the stimulated area eventually restores. This is normal chain of events triggered by the skin stimulation. There are two possible pathological outcomes of DT: long-lasting white dermographism and excessive red dermographism.
Long-lasting white dermographism is sign of increased activity of the sympathetic nervous system in the stimulated area. In such case the white line does not turn red quickly enough. The excessive red dermographism is sign of overactivity of the parasympathetic nervous system. In these cases, the white line turns red within normal time table but the red line increases to the way that stimulated area sometimes becomes edematous.
For our discussion, the case of long-lasting white dermoraphism is critically important. As we just mentioned in the case of long lasting white dermographism, the white line, which forms on the skin after its stimulation doesn’t turn red and in some cases continues to increase in size. You may see this phenomenon on patients with peripheral nerve neuralgia. For example, on the back of the leg in cases of Sciatic Nerve Neuralgia.
We may use the patient with long-lasting white dermographism as exact analogy of what is going on with the circulation in the area of active trigger point in the skeletal muscles. In both scenarios (i.e., white dermographism and active trigger point) there is local vasoconstriction as a result of increased activity of the sympathetic nervous system.
To demonstrate the phenomenon of long-lasting white dermographism, we filmed DT on one of our patients with Sciatic Nerve Neuralgia (see video below). Despite the very visual white dermographism reaction it was difficult for us to capture it on the video. This is why we try to pay attention to the slightest difference in skin color in the presented video.
Long lasting white dermographism on the posterior leg of the patient with Sciatic Nerve Neuralgia
At the beginning of the video you may see that we stroked the skin on the posterior leg three times and got a white lines that did not turn red and even started to widen. In the next part of the video, we compressed skin in one area of white line between thumb and index fingers. We kept the skin compressed just below pain threshold for half a minute. In the final part of the video we released compression while white lines above the compressed area were still clearly visible. At this moment you may observe that the compressed skin starts to turn pink (white arrow) while the rest of the white line did not change color at all.
This test recreates the exact chain of events during the application of ischemic compression in the area of active trigger point. By compressing the skin with visible signs of local vasoconstriction, we additionally deprived oxygen delivery to the compressed areas. After compression stops, reflex vasodilation was triggered (white arrow) as a response to temporary hypoxia caused by our compression. At the same time, the other parts of the white line did not change their color because the vasoconstriction is still raging there.
There is no doubt if one will stroke the area of the white line as suggested by proponents of the deep-stroking massage only he or she will get the same vasodilation effect while other parts of the white line are still affected by vasoconstriction. However, our goal was to prove that ischemic compression in the area with already compromise circulation was able to trigger reflex vasodilation as a result of pure compression.
The mechanisms which are responsible for vasodilation as a result of deep stroking and and as a result of ischemic compression are quiet different. In the first case the practitioner obtains the vasodilation as a result of mechanical effect while in the second case the reflex mechanism of the vasodilation is used. This is why deep stroking and ischemic compression should never be measured against each other. They are two equally important components (plus muscle energy techniques) of a scientifically sound protocol of TPT. As we discussed in Sept/Oct 2009 issue of JMS, the application of the ischemic compression in combination with deep pumping strokes and permanent fixed vibration allows optimized treatment by using local and reflex mechanisms of vasodilation during the same treatment session.
Conclusion: We hope that the scientific data presented in this article placed the four concepts we mentioned at the beginning of the article finally at rest. For the most stubborn believers this or any other source of scientific information will not change their beliefs, and we are powerless in those cases. For the rest of the readers, we would like to emphasize that fragmentation of the profession is a dead end. The clinically effective practitioner must see the larger and more integrative picture for the clients’ and patients’ health benefits, he or she must base their practice on scientific data rather than on the personal opinions and always challenge any new concept before applying it to the client or patient.
Hoheisel U., Mense S., Simons D. G., Yu X-M. Appearance of new receptive fields in rat dorsal horn neurons following noxious stimulation of skeletal muscle: a model for referral of muscle pain? Neuroscience Letters, 153:9112, 1993.
Korthuis R.J. Skeletal Muscle Circulation. San Rafael (CA), Morgan & Claypool Life Sciences, 2011.
Landmann H.R. “Trigger areas” as cause of persistent chest and shoulder pain in myocardial infarction or angina pectoris. J Kans Med Soc., 50:69-71, 1949.
Mackenzie J. Angina Pectoris Henry, Frowde & Stroughton, London, 1923.
Muscolino, J. Understanding and Working With Myofascial Trigger Points. MTJ, Spring, 1-5, 2008.
Nothnagel H. On neuritis in relation to its diagnosis and pathology. In: Clinical lectures on subjects connected with medicine, surgery and obstetrics by various German authors. Edited by R. Voikniann, London, New Sydenham Society, 201-36, 1877.
Quinter J.L., Cohen M.L. Referred pain of peripheral nerve origin: an alternative to the “myofascial pain” construct. Clin J Pain, Sep;10(3):243-51, 1994.
Schade H. Untersuchungen in der Erkaltungstrade: III Uber den Rheumatismus, in besondere den Muskelrheumatismus (Myogelose). Munch Med Wschr, 68, 95-99, 1921.
Rinzler S.H., Stein I., Bakst H., Weinstein J., Gittler R., Travell J. Blocking effect of ethyl chloride spray on cardiac pain induced by ergonovine. Proc Soc Exp Biol Med, 85:329-33, 1954.
Simons D.G. Cardiology and myofascial trigger points: Janet G. Travell’s contribution. Tex. Heart. Inst. J., 30(1):3-7, 2003.
Simons D.G. Letter to the editor. J. Man Manip Ther., 15(3):E69-70, 2007.
Travel J.G., Simons D.G. Trigger Point Manual, Wilkins&Williams.
Category: Medical Massage
