The purpose of this section of the Journal of Massage Science to inform the practitioners about valuable articles that frequently go unnoticed, as well as to point to those authors and publications who exhibit low educational standards. We do not play politics and we are not associated with any publishing company or professional association. We are a completely independent voice and we promise you direct unbiased reviews based strictly on the science.
If the author of the reviewed article does not agree with our opinion, we will be more than happy to publish his or her response and have a productive discussion over the article’s subject.
At the end of the year we will recognize and reward the author of the most important publication(s) and point to the authors of the most unscientific publication(s). We hope this will help to raise the bar of published materials in massage journals for the benefit of the entire profession.
Massage





How Does Pregnancy Changes a Female Client’s Body? Massage 155:50-53, 2009, by Kate Jordan
Great article! The author enumerated almost all possible somatic abnormalities, which the practitioner may encounter in female’s body after the childbirth.
The only our minor disappointment is the article’s format. Because of the importance of the subject for the clients as well as for the practitioners, we think the author should emphasize each possible abnormality separately maybe by using bullets instead “If your client…” approach.
As published, the article may go unnoticed by the readers. This format diminishes the importance of the subject as well as the author’s contribution.
We highly recommend that practitioners who work on female clients after childbirth make a copy of this article and underline each somatic abnormality separately to see the entire picture. In such case, the practitioner may systemize the information for better practical use in the future.



Effective Pain Relief. Neuromuscular Therapy. Massage 155:62-67, 2009, by Judith DeLany
The author gives a general review of the Neuromuscular Therapy (NMT) as well as explaining the differences between what she calls the European and American versions. She correctly presents basic principles of NMT, usage of the various massage techniques, sequence of their application, rules of pressure application, etc.
The article’s goal is to give the readers the general overview of NMT, but what surprised us is the complete absence of information on the importance of involving the client’s central and peripheral nervous system into the treatment.
From reading the article, the reader gets a very simple picture of NMT treatment: the client has a pain > the practitioner does assessment > finds the tight band and trigger point > he or she applies set of NMT techniques (gliding strokes, compression stretching, etc.) > the client obtains pain relief. We wish that it were so simple! Yes, such one sided approach will bring pain relief or even take care of a newly developed somatic abnormality. However, it will never completely eliminate somatic pathology if the client has a long-lasting, chronic case.
What is the difference? The difference is that in two to three weeks of suffering from the somatic pain, the body forms so-called reflex zones, which require a different approach to the therapy wherein the client nervous system needs to be engaged in an equal degree.
Let us give the reader the following example. Let’s consider that the client suffers from the chronic pain under the scapula, and the practitioner diagnosed the active trigger point in latissimus dorsi muscle. According to the author’s recommendation, the practitioner should work in and around the affected area addressing the tight bands and trigger point founded during the evaluation of the tissue.
However according to the established science of the NMT, the practitioner should start to work on the lower cervical area (C6-C8) segments because these are levels are where the latissimus dorsi muscle receives innervation. Next, the practitioner works along C6-C8 dermatomes as well as on other muscles (e.g., supraspinatus, infraspinatus, teres major muscles) innervated by the C6-C8 segments of the spinal cord. Only after all of this, should the practitioner work locally on the hypertonic muscle abnormalities in the latissimus dorsi muscle itself by addressing tight bands and trigger points.
This is of course a very general overview but it is how the treatment should be applied if the practitioner plans to rely on the healing power of the central and peripheral nervous system. Only gradual elimination or prevention of the reflex zones formation in combination with the local treatment gives the practitioner the stable clinical result.
Let’s look on the name of the modality: Neuromuscular Therapy. The information in the article reflects part of the method associated with word “muscular”, but contains nothing associated with the word “neuro”. Of course, the local treatment has impact on the entire body, but there are reflex zones or reflexes in the soft tissue the practitioner MUST address during the treatment separately. This is what gives the NMT its real healing power. While using the local treatment alone, the practitioner flies with the one-winged NMT, while combining the local and reflex principles of NMT the practitioner uses two powerful wings to support his or her therapy.
Final words regarding the differences between views of Dr. L. Chaitow and the author: The differences are not in the pressure or in the nature of the gliding strokes the author mentioned but that in every publication Dr. Chaitow stresses the importance of the nervous system and its role in the NMT while the author misses this part of NMT completely (at least in this article).
The author tries to describe her variant of the trigger point therapy, which is always the integrative part of the NMT. However, her description based on the very simple assumption; the practitioner detected the painful spot or nodule, and just applies the direct vertical compression on it until, “…the practitioner feels a softening of the compressed nodule”.
This recommendation does not have anything to do with the science of massage therapy. The best outcomes of the authors’ recommendations are transfer of the trigger point in the latent or sleeping state.
Massage Today





Incorporating Lymphatic Drainage in Facelift Massage. Massage Today, 9(4), 2009, by Rita Woods, LMT
In difficult financial times, new sources of referral for massage practitioners are priceless opportunities to increase their business. The implementation of Lymph Drainage Massage (LDM) as a new service for clients who want to use it for cosmetic purposes is a significant extension of the services in the spa or private massage clinic. Thus, the topic is of great importance to the profession.
The author shows that she understands the general concept of LDM, its mechans and contraindications. She correctly identifies two key areas for lymph drainage from the face: terminus and submandibular lymph nodes.
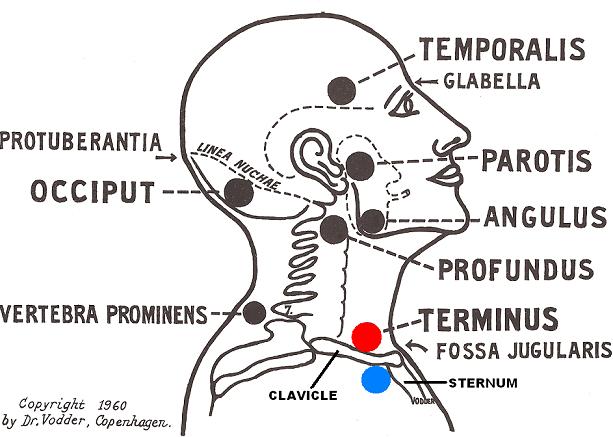
The term “terminus” was proposed by the inventor of LDM, Dr. E.Vodder, in 1936. The terminus is not an anatomical structure but rather the place of application of the LDM techniques in the areas where the thoracic duct curves on the left side before it empties into the venous system and the right lymphatic duct formed on the right side of the neck.
In the final part of the article, the author offers the protocol of LDM, which should be used in cases of Facelift Massage. That is where the entire article loses credibility. Let us quote the protocol:
“1. Warm the facial muscles using any gentle, non-invasive technique
2. Gently stimulate the lymphatic terminus which is found below the clavicles and on either side of the manubrium (i.e. upper part of the sternum)
3. Stimulate the submandibular lymph nodes by using digital pressure up underneath the mandible bone
4. Proceed with your facelift session protocol”
According to Dr. Vodder and International Society of Lymphology, the terminus are located in both supraclavicular areas (i.e., above the clavicles). The application of LDM as the author recommends “…below the clavicles and on either side of the manubrium” will produce the same effect on the lymph drainage from the face as the application of similar techniques on the client’s foot.
It is anatomically, physiologically and clinically impossible to affect lymph drainage through the terminus below the clavicles and next to the sternum because the upper ribs make terminus inaccessible. This recommendation is not just a small mistake or inconsistency it is completely erroneous and will negate all efforts by the practitioner if he or she were to follow such advice.
Even the name of the LDM technique to address the terminus is Supracalvicular Pump. However, to eliminate any doubts in this controversy, we invite the readers to examine Dr. Vodder’s original drawing of the treatment points for the LDM on the neck and face (see Fig. 1). We marked the correct location of the terminus by a red dot and the author’s incorrect recommendations by a blue dot. The small difference in the location of treatment area is significant to the practitioner and client.
After working in the area of the terminus, the author recommends to move to the submandibular lymph nodes. In the beginning of the article, the author correctly states that: “As with any ‘waste disposal’, some form of clearing should be done before adding more waste to the system”.
However, the author contradicts herself because before draining submanibular lymph nodes the practitioner MUST drain the lymph nodes on the anterior neck. Only after draining the anterior neck can the practitioner address the submanibular lymph nodes. Otherwise, drainage of all waste products will be blocked on the level of anterior neck that was not cleaned before upper segments are added. Ironically, enough the picture in the article clearly shows the abundant locations of the cervical lymph nodes on the anterior neck (between submandibular lymph nodes and terminus), the same nodes the author completely disregarded.
At the end of review, we would like to quote Dr. E. Vodder (Paris, 1936): “Stagnation of the lymph flow, therefore has catastrophic results for health and beauty: one must get the lymph circulation going again at all cost and this is achieved with the help of manual lymph drainage” We can guarantee that such drainage will be greatly compromised if the practitioners will use the protocol recommended by the author.
The final question should be addressed to Massage Today. Is there any review procedure by the Editorial Board where incorrect information may be stopped before it is published and recommended to the massage practitioners?





Tools to Succeed for Massage Therapists. Massage Today, 9(5), 2009, by David Kent
Great article! In the beginning of the article, the author poses the following question: “In these tough economic times how can you stand out above the competition so that clients will continue to spend their time and money on treatments with you?” From our point of view, it can be done by learning and practicing the medical aspects of massage therapy and also following the guidelines provided in this article. Scientifically based communication with the client in the same degree as a treatment itself will build your practice.




The Progression of Airway Obstruction. Massage Today, 9(5), 2009, by Dale G. Alexander, LMT, MA, PhD, Thomas M. Walsh II, DDS
Very good, and scientifically grounded article. This article definitely should be read by massage practitioners. They should keep this information in mind when working on clients with TMJ dysfunction or with tension in the cervical muscles. The only disappointment in the article is a complete lack of practical recommendations for the practitioners.




New Perspectives on ITB Friction Syndrome. Massage Today, 9(5), 2009, by Whitney Lowe, LMT
Great article! We believe every article must enrich the reader and provide him or her with new information. The massage practitioners rely mostly on the professional publications, which very frequently become free advertising for authors’ books, DVDs or seminars. We hope in the future, we will enjoy articles like this one in every major journal.
However, we disagree with the author on one issue. The findings of the Fairclough, et al.(2006) do not diminish the clinical value of the friction applied on the ITB on the lateral side of the knee. The author is completely correct when he points out that the treatment of ANY pathological abnormality of the ITB must start at the tensor fascia latae and gluteus maximus muscles. They are keys to the tension in the ITB. The MEDICAL MASSAGE PROTOCOL in our Video Library emphasizes exactly the same approach.
Those who advocated the usage of local treatment of the ITB pathology alone are completely wrong. However, the notion that after the publication of the Fairclough, et. al. article the practitioners need to abandon the local treatment and switch completely to the tensor fascia latae and gluteus maximus is equally incorrect. Lets don’t throw out the baby with the bath water.
We believe that at the end of the session the practitioner MUST apply cross-fiber friction on the lateral side of the knee because the irritation of the richly innervated fatty tissue will secondary produce low grade inflammation in the periostreum of the femoral and tibial epicondyles as well as the fibular head. There is no more efficient local therapy for these abnormalities as the periostal massage, and cross fiber friction is one of its techniques.
Thus the clinical success is a result of the combination of both treatments, and this is what the MEDICAL MASSAGE PROTOCOL is based on.



Prevention and Rehabilitation of Conditions Leading to Hip Replacements.Massage Today, 9(5), 2009, by Don McCann, MA, LMT
Overall, this is a good article. The author correctly states that before the physician and client consider the hip replacement surgery they should give the massage practitioner a chance to work on the client with correct protocol even if there is significant destruction of cartilage. It is a medical fact that elimination of the spinal or peripheral nerve irritation as well as correct alignment of the femoral head in the acetabulum may eliminate even debilitating pain in the hip joint without the surgery.
However, we do not agree with the some theoretical and clinical aspects of the article. The author constantly mentions pelvic imbalance as a result of “anterior/posterior rotation of the iliums”. We do not know where the author found separate ilium’s rotation without mentioning the entire pelvis. If we consult any modern anatomy text book, we will find that:
1. The ilium is FUSED with ischium and pubis bones to form one solid bone structure called the pelvis. This fusion is a major reason for the pelvis’s rigidity and stability. If we consider that the pelvic bones wiggle against each other, we are in great danger of misleading ourselves and undermining the entire concept of body balance and role of pelvis. There is no movement between three of these bones (on each side of the pelvis).
2. The ilium forms the sacro-iliac joint with the sacrum. Because there is no synovial cavity within the SI joint. There is a very little movement in this joint. However, “Movement at this joint decreases with the age and ankylosis (i.e., full fusion of the joint, JMS) is complete by age 50″ (E.W. April. Medical Anatomy).
As we understand from the medical literature and personal clinical experience, hip replacement surgery is very rarely performed before or around age of 50 (except of severe trauma). In such case, what exactly anterior/posterior rotation of the ilium has the author detected in his clients considering the fact that such rotation is not possible?
If we accept that modern anatomy texts are correct, the author’s statement about the ilium’s rotation becomes groundless because the ilium will rotate only if ENTIRE pelvis (i.e., both iliums, both ischial and pubic bones as well as the sacrum) is rotated.
Even more puzzling is the notion that the author was able to eliminate such non-existed ilium rotation. So how in such case, has the author helped his clients avoid surgery or assist in their rehabilitation? Everything is much simpler: there is no such thing as anterior/posterior rotation of the ilium and the author worked on the lower back muscles (especially quadratus lumborum muscles) and gluteal muscles.
As result of restoration of their anatomical length, elimination of the residual tension, restoration of normal resting muscle tone and elimination of the condition of the hyperirritability of the muscle spindle receptors and the balance (which is controlled by muscle tension) of the entire pelvis was improved. It unloaded the overstressed cartilage of the acetabulum and femoral head and intensity of the hip pain subsided.
In another therapeutic scenario of the author’s therapy, he eliminated the irritation of the spinal or peripheral nerves, which innervated the hip joint and that in turn liquidated the pain in the hip joint.
A couple of final words for this review. The deep tissue massage techniques recommended by the author should not used on the older clients. The same results can be achieved with much more gentle protocols without excessive digging into the fragile soft tissue of aged clients. The practitioner should work just below the client’s personal pain threshold and constantly correlate applied pressure with his or her pain sensations.
Massage Therapy Journal




Body Language. Massage Therapy Journal, 48(1), 2009, by Clare La Plante
The article covers a very important topic: How to prevent professional injuries. This article is helpful for the practitioners because it makes them more in tune with their own body and enforces important message. When you feel pain, it already means you missed an important time when simple measures (rest, hot bath, treatment from other practitioner, etc.) were able to prevent injury. Unfortunately, the body shows very small signs, and we frequently don’t pay attention to them until it is too late.
The only disappointment is the article’s format. It enumerates potential problems and ways for self-help but it does not give the reader a clear framework for what do and what to avoid.





Building Blocks. Massage Therapy Journal, 48(1), 2009, by Jolie Haun, LMT, PhD
Rare example of real scientific article in modern American massage literature. More research and more articles like this one and the place of massage therapy in the American society and medicine will change.





What is Muscle Memory? Massage Therapy Journal, 48(1), 2009, by Joe Muscolino, DC
Great and informative article! In the most simple language, Dr. Muscolino explained the concept of the muscle memory and informative illustrations are great help.
Why the subject is important? Many times during seminars or lectures, the members of our Editorial Board face questions about muscle memory and in many cases, to our surprise, the massage practitioners thought that muscle memory is the natural ability of the muscles to store previously learned patterns of contraction.
In some cases, the situation even gets worse because there are “educators” who use the scientific concept of the muscle memory and somehow link it with suppressed memories, subdued emotions and even past-life experiences. In their skillfully manipulative hands, the scientific concept becomes link to the world of supernatural.
Dr. Muscolino correctly explains the nature of muscle memory as a physiological and scientifically grounded concept. It is up to practitioners to decide between the science and occult teachings.
We don’t want the readers to get the impression that the client’s mental and emotional states don’t have an impact on the somatic system. We would like to emphasize that the emotional state of the client as well as his or her personal life experiences and memories indeed affect the resting muscle tone and body posture. However, this does not have anything to do with the muscle memory, which some assume secretly to exist in the muscles themselves.
Category: Good Apples, Bad Apples
