by Ross Turchaninov, MD and Boris Prilutsky, MA, LMT
In the first article we briefly reviewed the history of the trigger point concept as well as major mechanisms of the trigger point formation. This part of the article is dedicated to the examination of the trigger points and their differentiation.
TYPES OF TRIGGER POINTS
One of the most common mistake practitioners make is to believe that trigger point is a pathology associated with the skeletal muscles only. From book to book and from article to article we see authors discussing the trigger points in the skeletal muscles and various approaches to their treatment without even mention the fact that trigger points may develop in three types of the soft tissue: skin (cutaneous trigger points), skeletal muscles, and perisoteum (periostal trigger points).
In many cases the practitioners don’t consider “other” trigger points important or having clinical value for the simple reason that this essential part of massage science was never taught in the massage school and very rarely mentioned in the publications or during the educational seminars.
In the real life, in massage therapy room, the practitioners encounter the clients with active trigger points in each type of the soft tissue on daily basis without even considering to include all of them into the treatment protocol. This factor alone makes the practitioner less effective and this is why he or she will eventually loose the client(s) which will be disappointed by the lack of the progress in the treatment.
Despite that the subject of this article is trigger points in the skeletal muscles we would like at least briefly to introduce the reader to the trigger points in the skin and periosteum because the correct differentiation between them and trigger points in the skeletal muscles is an essential component of the successful somatic rehabilitation.
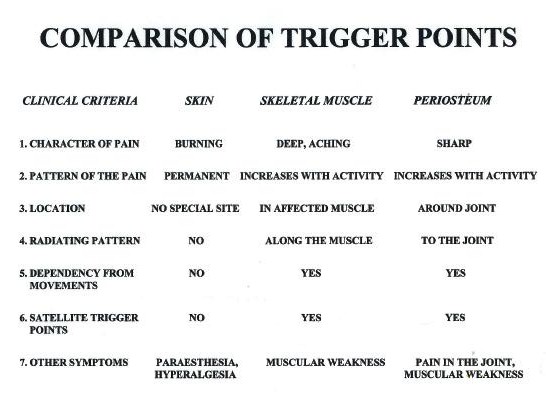
Everyone who practices the somatic rehabilitation must keep in mind this very simple table (see Fig. 1) which allows you easily even during the client’s questioning to figure out if other types of the trigger points play role in the client’s pathological symptoms.
Fig. 1. Clinical differentiation of trigger points
Cutaneous Trigger Points
The cutaneous trigger points were extensively studied by D.C. Sinclar, MD in 1948-1949. The major clinical sign of the cutaneous trigger points is combination of the pain and burning sensation on the skin. Sometimes client may tell you he feels as someone placed hot coin on the part of the body. This burning pain frequently accompanied by surrounding sensation of tingling.
If the cutaneous trigger points are present they are sign of the nerve irritation. For example the client has Sciatica and as a result of sciatic nerve irritation the cutaneous trigger points may form on the leg or foot. However much more frequent scenario is formation of the cutaneous trigger points on the upper and middle back as a result of irritation or compression of the cutaneous branches of the spinal nerves responsible for the innervation of the skin on the upper back.
The very frequent mechanism of cutaneous trigger points formation on the upper back will have the following chain of event. The client works a lot on the computer and for hours keeps head in the steady position concentrating vision in one spot. As a result of excessive isometric work by the trapezius muscle it develops the tension and its resting muscle tone increased. The cutaneous nerves after they branched out from the spinal nerve passing through the fibers of the trapezius muscle before they appear under the skin to innervate it. Fig. 2 shows the cutaneous branches of the spinal nerves on the neck an upper back. The tensed trapezius muscle squeezes cutaneous nerves and as a result cutaneous trigger points will form in the part of the skin innervated by the compressed or irritated cutaneous nerve.
Fig. 2. Cutaneous branches of the cervical and thoracic spinal nerves
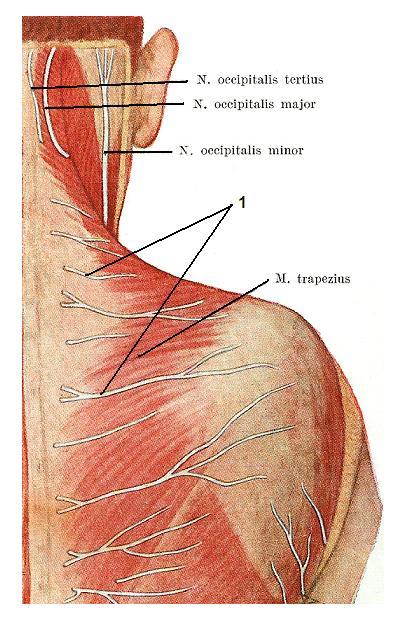
1 – cutaneous branches of the spinal nerves
Periostal Trigger Points
The concept of periostal trigger points as well as Periostal Massage to treat them was developed by two German physicians Dr. P. Vogler and Dr. H.Kraus in 1940es.
The periostal trigger points formed in the periosteum. The periosteum is the connective tissue membrane which covers the outer surface of all bones and is tightly connected with them. The periosteum is the major source of bone metabolism and innervation and it is the place where all tendons, ligaments, fascia etc. insert into the bones.
The periosteum is a very richly innervated membrane and trigger points when they form in the periosteum are very painful. As a matter of fact the periostal trigger points are the most painful ones. The clients with acute Tennis Elbow, Golfer’s Elbow, De Quervain’s Disease etc., will tell you that every even small movement of the affected joint produces excruciating pain.
The high intensity of the pain around the joint triggered by active movements and accompanied by muscle weakness are clinical signs of periostal trigger points (Vogler, Krauss, 1953).
Why the practitioner should know and differentiate trigger points? First of all the trigger points may and frequently are coincides with each other. For example, the active trigger point in the levator scapulae muscle frequently accompanied by cutaneous trigger point located directly atop of the muscle trigger point and at the same time the periostal trigger point can form closely in the perisoteum of upper medial angle of the scapula.
If the practitioner wants to get stable clinical results and help the client he or she should address each type of the trigger point with the specially designed techniques (e.g., superficial friction and skin kneading for the cutaneous trigger points and periostal massage for the periostal trigger points). Here we will discuss the evaluation and treatment of the trigger points in the skeletal muscles.
CLASSIFICATION OF THE TRIGGER POINTS IN THE SKELETAL MUSCLES
The critical part of evaluation of the skeletal muscle is finding the location of trigger points and understand their nature. Let’s start with the definition of the trigger point. Despite the fact that the client feels the trigger point as a pain with a pin-point location, the area of the muscle which carries the trigger point isn’t in a round form, but can be best described as having a spindle- like form within the muscle tissue. Thus, trigger point is a part of the hypertonus where a number of the muscular fibers exhibit the strongest spasm. This spasm is a fundamental cause of trigger point formation because it diminishes blood circulation through the affected tissues (Fassbender, Wegner, 1973; Popelansky et al., 1976; Travell, Simons, 1983, etc.).
According to the world wide accepted classification (Travel and Simmons, 1983) the trigger points in the skeletal muscles separated on:1. Active trigger point (ATP)
2. Latent or “sleeping” trigger point (LTP)
3. Satellite or referred trigger point (STP)
4. Secondary trigger points (SCTP)
5. Motor trigger point (MTP)
6. Tender points (TP)
1. Active trigger point (ATP)
The ATP(s) hold the key to the muscle tension and pain in the affected area. ATP is the area of the greatest pain felt by the client during active movements or while the practitioner applies direct pressure on it.
The ATP forced the client to start looking for help. This trigger point is an epicenter of acute pain. The pain from the ATP usually radiates along the fibers of the same muscle or along the entire muscle group.
Another important symptom to remember is muscle weakness. A muscle with ATP becomes weak to the degree of being unable to execute motor commands from the central nervous system.
ATP in every skeletal muscle have the tendency to form in the same areas. This is why the map of trigger points is a helpful diagnostic tool.
2. Latent or “sleeping” trigger point (LTP)
LTP is an active trigger point which, as a result of self-treatment or inappropriate professional treatment, was not eliminated but transferred into a so-called “sleeping” state.
The LTP does not bother the client either during physical activity or during the rest, but is the major cause of stiffness (especially in the morning). Muscles which harbor LPPs are easily fatigued, and weaker. LTPs may also trigger moderate pain at the very end of movement.
LTP can be easily reactivated and become active ones and vice versa. In a sense, the LTP is the chronic presence of the condition of hyperirritability of the muscle spindle receptors. Thus, reactivation of the LTP can be caused by any factor, from physical overload to changes in the surrounding temperature. The constant transition of the active trigger point into the latent state and back is the major cause of the formation of the core of myogelosis.
3. Satellite or referred trigger point (STP)
STP are also painful areas of muscular tension. However, the intensity of the pain is less and they are smaller. STPs also contribute to the overall muscular weakness, pain, and tension.
The patient does not feel STPs the same as he or she feels active ones. They are mostly felt as a radiation of the pain from the active trigger point (Jacobs, 1960; Popelansky, et all, 1976; Travell, Simmons, 1983). Thus, to detect the location of the STP, the practitioner has to ask the patient about the patterns of the pain radiation from the active trigger point, and examine these areas.
4. Secondary trigger points (SCTP)
All muscles which are responsible for movement in the joint are separated into “prime movers” and “synergists”. A prime mover is the muscle mostly responsible for this particular movement in the joint. Muscle synergist helps the prime mover when extra force is needed for the specific tasks. For example the prime mover of the elbow flexion is biceps brachii muscle, but synergists of the same movement are brachialis and brachioradialis muscles.
SCTPs are formed in the muscles-synergists as a result of their overload. If biceps brachii harbors an active trigger point it becomes weaker and it is unable to provide all the necessary force for the flexion of the elbow on its own. In such a case, the brachialis and brachioradialis muscles start to work harder. However, they were not designed to be prime movers. Both muscles are supposed to work only as assistants. Now they have to participate in every flexion of the elbow. As a result of their overload, secondary trigger points start to develop.
5. Motor trigger point (MTP)
Some authors (Gunn et all, 1976; Travell, Simons, 1983) also separate the so-called motor trigger points. MTPs are located in the areas of neuro-muscular junction where the motor nerve which innervates the muscle enters it. Several studies on the subject of MTPs showed that in these areas the strongest muscular contractions are registered if the weakest electric current was applied. In any case, the authors use the terms “trigger points” and “motor points” interchangeably.
Why MTP are formed in the areas of neuro-muscular junction in some cases and they are not present in other cases? Usually MTP are secondary reaction to the nerve irritation or chronic muscle and fascia tension. According to histologically conducted studies (Heine, 1997; Gogoleva, 2001) chronic pain and low grade tension in the skeletal muscles and fascia are responsible for the low grade inflammation around the terminal parts of motor nerve which ends at the neuro-muscular junction. This chronic inflammation activates the local fibroblasts, which deposit collagen around the nerve endings forming so-called “collagen cuffs”. These “collagen cuffs” detected around the neuro-muscular junctions interfere with very intimate neurochemical process of transferring impulse from the nerve tissue to the muscle tissue. This mechanism is responsible for the generation of pain in the area of MTP(s).
MTPs have very unique diagnostic value. According to several studies, the abundant presence of motor trigger points is a sign of spinal nerve irritation or compression by the bulging disk or other structures in the area of the vertebral segment (Gunn et all, 1976). Always keep this in mind.
6. Tender points (TP)
Patients with Fibromyalgia have a different type of trigger points which are called tender points. This is subject of another discussion and we will review it in one of future issue of our Journal.
EVALUATION OF THE TRIGGER POINTS IN THE SKELETAL MUSCLES
As we just discussed above there are several types of the trigger points in the skeletal muscles. In very complicated, chronic cases of the long existing muscle pathology several types of the trigger points may co-exists at the same time and this is the most confusing part of TPT.
Let’s simplify as much as possible the subject of evaluation of the trigger points. We will provide you very simply and effective tests and diagnostic techniques which you may start to use in your massage room immediately.
Evaluation of Active Trigger Points (ATP)
ATP is the most painful symptom of the muscle tension. It is critically important to detect the ATP at the very beginning. It is relatively simple task if the client has fresh case and ATP is single. The situation becomes much more difficult if the practitioner deals with the chronic muscle pathology. In such case the satellite, secondary or motor trigger points complicate examination and frequently mislead the practitioner.
The earliest detection of the ATP is a must because it frequently holds the key to entire tension in the affected area. If the practitioner made incorrect decision and addressed secondary trigger point instead of the ATP he or she fights with windmills.
How to detect ACT:
1. Questioning
Ask the client to pinpoint the most painful area and after this ask him or her to show you movement which triggers the most intense pain in this area. Match this information with the map of trigger points.
2. “Jump Symptom” Test
There is a limited number of diagnostic tools to evaluate hypertonic muscular abnormalities and the “Jump Symptom” is still the most effective one (Fisher, 1988). Always start with palpation of the affected area using pressure just below the threshold of pain. Try to detect structural changes (e.g., dense areas, tight bands, etc.) within the examined muscle. Ask the client to report any pain sensations and their intensity during the examination. After this, apply pressure above the threshold of pain in the suspected areas.
If the examiner hits a trigger point, the client will feel acute pain and react with the so called “jump symptom” which is withdrawal of the examined segment or entire body from the practitioner (Kraft, et all 1968).
The video shows the application of the Jump Test on ATP’s in the trapezius muscle. In the beginning of the video, the black dot indicates the most common location of the ATP in the lower portion of the trapezius muscle. The second part of the video shows the client’s reaction to the Jump Test.
All videos in this article are from our Video Library of MEDICAL MASSAGE PROTOCOLs.
3. Movement Test
If the client has a new case of hypertonic muscular abnormality with one trigger point and one affected muscle, the diagnostic evaluation is an easy task. The situation becomes much more complicated when the hypertonic abnormality has a long history and there is a clinical picture of widespread pain and muscle tension. In such cases, the application of pressure on any area along the affected and neighboring muscles will produce the “Jump Symptom”. However, as we discussed above, the ATP must be treated and eliminated first. How can practitioner differentiate between trigger points in hope of finding the active one if each of them produces pain of the same intensity? The Movement Test is specially designed for these cases. It is very simple and informative.
The video shows the application of Movement Test on the right shoulder. The client has chronic Deltoid Muscle Syndrome.
Ask the client to perform movement in the joint or part of the body which causes the pain (shoulder abduction in the video). Now, press finger in the area being examined and ask the client to repeat the same movement. If the practitioner presses into the ATP the client will be able to repeat the same movements without pain or with a very tolerable amount of it as long as the practitioner maintains the compression of the tissue (see second part of the video). As soon as the practitioner releases the finger and asks the client to repeat the same movement, he or she will feel the pain again and stop movement as soon as the critical level of contraction is reached (see third part of the video). In other words, the practitioner uses pressure to deactivate the ATP, and as long as it is deactivated, the muscle is able to productively contract.
If the practitioner examines the satellite trigger point instead of the ATP the patient will still have pain in the tested muscle during its contraction despite the fact that the practitioner is maintaining the compression of soft tissue (see fourth part of the video). Thus, the Movement Test allows to differentiate between various types of trigger points and to find the active one quickly.
Evaluation of Latent Trigger Points (LTP)
The client who has LTP never complains about pain or uncomfortable sensations in the affected area. The most he or she will mention is morning stiffness which usually disappears in hour or two.
The only way the practitioner may detect the LTP is a “Jump Symptom” Test. If the practitioner applies pressure in the LTP the client exhibits classical reaction of body withdrawal and this pain disappears as soon as the pressure ceases. Usually the clients very surprise to feel pain in these areas because they never bothered them. If LTP present this area(s) must be included into the treatment protocol and LTP should go through the same therapy as ATP.
Evaluation of Satellite Trigger Points (STP)
STP is easy to find as soon as practitioner determines the ATP. The practitioner should ask the client about any pain radiation. If the pain radiates to the distant areas, for example ATP in the pectoralis major muscle accompanies by the radiation of the pain to the hand, the practitioner can be sure that he or she deals with the radiation of the pain along the peripheral nerve. However if the client complains about radiation of the pain from the anterior surface of the shoulder joint to the anterior chest the practitioner can be sure that this pathway of the pain radiation is associated with the APT in the pectoralis major muscle.
The best way to examine muscle on the presence of STP is to apply pressure along the pathway of the pain radiation which client showed you during questioning. Usually during the application of pressure the clients do not exhibit classic jump sign because intensity of the pain is much less in the STP(s). Also, remember or record the location of STP because they need to be completely deactivated during the treatment.
The video below shows the evaluation of STP(s) formed along the pathway of pain radiation from the active trigger point in the middle portion of the deltoid muscle.
The black dot represents the active trigger portion of the deltoid muscle. The small circle is the insertion of the deltoid muscle into the humerus. In the beginning of the video, the client indicates the pathway of pain radiation. In the second part the practitioner applies pressure along the indicated route, and correlates the pressure application with the client’s sensation of pain.
The final part of the video shows the location of two STP’s (x-symbols) detected in the middle portion of the deltoid muscle.
Evaluation of the Secondary Trigger points (SCTP)
SCTP is much more rare compare to all other types of the trigger points. Usually they formed when long lasting chronic muscle tension is present in the muscle prime movers. The palpation of muscle synergists is the only way to detect tension there.
The only problem with the muscle synergists that they are frequently located under the muscle prime movers. Thus to examine the muscle synergists the practitioner should be familiar with approach to mobilize the superficially located prime mover to get to the muscle-synergist directly without eliciting pressure on the superficially located muscle.
The video shows the practitioner mobilizing the gastrocnemius muscle (the prime mover) in order to examine the SCTP in the soleus muscle, which is the muscle synergist. We show the most common techniques of mobilization of superficial muscles in order to reach deep muscles in our video library.
Evaluation of the Motor Trigger Points (MTP)
MTP is very easy to examine with the application of the direct pressure in the middle of muscle belly. This is always area where motor nerve which innervate the muscle enters and forms the neuro-muscular junction. The MTP is always singular.
If the muscle has short tendon the detection is MTP is a very easy task. The practitioner looks on the places of muscle origin and insertion and in the middle of this line he or she should apply vertical pressure to determine if the MTP is active. The video shows the detection of the location of the MTP in the middle of the lateral head of the triceps brachii muscle.
If the muscle has a long tendon, the practitioner should remember that the MTP is located in the middle of the muscle belly. For example, the extensor digitorum muscle has a long tendon which insets into the phalanges. However, the actual belly muscle is very short, and the MTP, if it is active, is located in the middle of the muscle.
The video shows the MTP located in the middle of the muscle belly of the extensor digitorum muscle.
Compass Technique
Let’s consider that you detected the presence of ATP and STP in the client and you are ready for the trigger point therapy. However before you start you need one last piece of information otherwise your treatment will be less effective. You need to detect the entrance into the trigger point. You can easily do it using so-called Compass Technique.
As we mentioned above the trigger point is a spindle-like area of tension which has 3-D orientation within the affected muscle and this orientation is always unique for each case. Because the trigger point is made up of a number of muscular fibers which are in spasm the “entrance” into the trigger point reflects the main orientation of these fibers within the affected muscle.
Why is the determination of the “entrance” into trigger point so important? This has a great impact on the following application of trigger point therapy. If the practitioner is able to detect the location of ATP as well as its “entrance”, he or she only needs to use a very small amount of pressure to produce effective ischemic compression. As a result, the already affected muscular fibers are not injured, the client does not generate protective muscle tension and the practitioner does not exhaust himself or herself during the application of ischemic compression.
The wrong concept of “no pain, no gain”, which is frequently applied to trigger point therapy, is a direct result of not knowing about this basic rule of trigger point therapy.
Let us illustrate the concept of the “entrance” into the trigger point with the help of Fig. 3.
Fig. 3. Detection of the entrance into the trigger point using the Compass Test
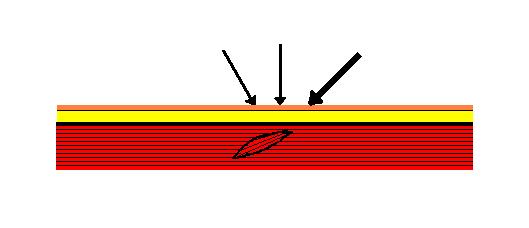
Tensed muscle fibers which form the trigger point are arranged in a particular direction. If the practitioner applies pressure in the trigger point from any of the directions as shown by the thin arrows, he or she will hit the area of the trigger point and the patient will report acute pain and sometimes show the “jump symptom”.
However, only the application of pressure in the direction shown as a thick arrow will produce extremely unpleasant and even stabbing pain, while the intensity of the pressure used remains identical. This is the “entrance” into the trigger point. The practitioner should remember the position of the finger and angle of the pressure application because he or she will use this direction during trigger point therapy.
The video shows the clinical application of the Compass Technique on the lower portion of the trapezius muscle (black dot). First explain to the client what you will be doing, as you will need his or her active participation. Tell the client that you will place your thumb onto the tissue and you that you will slowly increase the pressure until he or she starts to feel pain in the compressed area; and that as soon as your pressure reaches the pain threshold (the very first signs of discomfort), the client should immediately inform you about any pain he or she feels (in the video word: “Pain!”). Note the degree of pressure it takes to activate the pain receptors in the area of the trigger point when pressure is applied in this particular direction.
As soon as the pain threshold is reached, decrease the pressure to the level of light touch, and change the angle of the thumb. After having changed the angle, begin to slowly increase the tissue compression until you again reach the pain threshold.
The practitioner should repeat the same slow compression at different angles until he or she establishes the position of the thumb and angle of pressure application at which a given degree of tissue compression on the point will produce the most intense pain sensations (in the video phrase “Strong Pain!”). At once the patient will feel that pressure unchanged in terms of intensity but altered only in terms of the angle of its application produces a sharp, or even a stabbing, pain. This particular angle of the pressure application is the entrance into the trigger point. The practitioner will use this angle during the ischemic compression..
The last part of the video shows the position of the thumb at the entrance into the trigger point. The thumb position indicates the angle of the pressure the practitioner will use during the TPT. The white arrows in the video indicate different angles of the applied pressure during the application of the Compass Technique.
The application of ischemic compression at the angle established during the Compass Technique allows the practitioner to eliminate an active trigger point quickly and efficiently without transferring it into a sleeping state, or damaging muscle tissue to the point of myogelosis formation.
The last issue we would like to discuss in the second part of this article is usage of trigger point maps. They are extremely important tool for the evaluation of the trigger points. However they have their limitations and the practitioner can’t rely only on them. The map of trigger points don’t mentioned cutaneous and periostal trigger points and they show only approximate location of the trigger points. The later issue become very important because trigger points on the different levels are frequently located in the same area.
For example ATP in lower trigger point in the trapezius muscle is located almost exactly on the top of the ATP in the rhomoideus major muscle. Their evaluation demands different degree of pressure and the practitioner’s expertise to mobilize the trapezius muscle as more superficial one to get direct access to the more deeply located rhomboideus major muscle.
REFERENCESFassbender H.G., Wegner K. Morphologie und Pathogenese des Weichteilrheumatismus. Z. Rheumaforsch, 32:355-374, 1973
Fisher A.A. Documentation of Myofascial Trigger Points. Arch Phys Med rehab, 69, 286-291, 1988
Gogoleva, E.F. New Approaches to Diagnosis and Therapy of Fibromyalgia associated with Spondylosis. Ther. Arch., 4:40-45, 2001
Gunn C.C., Milbrandt W.E. Tenderness at Motor Points. A Diagnostic and Prognostic Aid for Lower Back Injury. J. Bone JT Surg, 58-A, 6, September, 1976
Heine, H. Lehbruh der biologischen Medicine. Stuttgart, Hippokrates, 1997
Jacobs M. Massage For the Relief of pain: Anatomical and Physiological Considerations. Phys Ther Rew 40(2):93-98, 1060
Kraft G.N., Johnson E.W., LaBan M.M. The Fibrositis Syndrome. Arch Phys Med Rehab, 49, 155-162, 1968
Popelansky Y.Y., Zaslavsky E.S., Veselovsky V.P. Medico-Social Significance, Etiology, Pathogenesis and Diagnoss of Extra-Articluar Pathologies of the Extremities and Dorsum Soft Tissue. Voprosi Reumatologii, 3:38-43, 1976
Sinclar, D.C. The remote reference of pain aroused in the skin. Brain 72:364-372, 1949
Travel J.G., Simons D.G. Myofascial Pain and Dysfunction. The Trigger Point Manual. Williams&Wilkins, 1983
Vogler, P, Krauss, H, Periostbenhandlung. Leipzig, 1953
For Dr. R. Turchaninov bio click here
Mr. B. Prilutsky, practices and teaches Medical and Sports Massage for more than 30 years. He has master degree in physical education and rehabilitation from Ukraine.
Mr. Prilutsky has worked with athletes and world dignitaries throughout Europe, Israel and USA. He is the founder of the Institute of Professional Practical Therapy in Los Angeles and to date, he has trained thousands of therapists world-wide. Boris Prilutsky has published extensively on various topics of physical medicine and rehabilitation.
Category: Medical Massage
Tags: 60 Variations of 7 Basic Techniques, Journal of Massage Science 2009 #3