The purpose of this section of the Journal of Massage Science to inform the practitioners about valuable articles that frequently go unnoticed, as well as to point to those authors and publications who exhibit low educational standards. We do not play politics and we are not associated with any publishing company or professional association. We are a completely independent voice and we promise you direct unbiased reviews based strictly on the science.
If the author of the reviewed article does not agree with our opinion, we will be more than happy to publish his or her response and have a productive discussion over the article’s subject.
At the end of the year we will recognize and reward the author of the most important publication(s) and point to the authors of the most unscientific publication(s). We hope this will help to raise the bar of published materials in massage journals for the benefit of the entire profession.
Our Editorial Board would like to introduce the Appreciation Award for the American massage publication which has contributed the most important articles to the science of massage therapy in 2009.
The trophy is made from polished brass on a marble pedestal with an exotic wood foundation and decorated with blue agate. Its dimensions: 10 x 8.8 x 8.8″ (25 x 22 x 22 cm).

The symbolism of the Appreciation Award: letter M indicates massage; the two serpents represent twin roles – preventive and medical – of massage; two serpents form the heart which represents love and compassion of our wonderful profession.
Our Editorial Board will present the Appreciation Award at the beginning of 2010.
Massage & Bodywork





The Forgotten Core. Revisiting Abdominal Massage. Massage & Bodywork, July-August, pp.72-79, 2009, by Marybetts Sinclar
This is an important article. Less and less massage practitioners include abdominal massage as a part of their stress-reduction or therapeutic massage session. Even smaller numbers of practitioners are able conduct the abdominal massage in cases of abdominal inner organ abnormalities.
We praise the author for her statement concerning insufficient education provided in schools on the subject of the abdominal massage: “…many schools increasingly de-emphasize its (abdominal massage) importance. Fewer class hours are spent on abdominal massage”, and “Some schools teach students that massage of the abdomen is an optional part of a full body Swedish massage”. Unfortunately these statements are correct.
The practitioner greatly reduce their impact on the client’s body by skipping the abdominal massage as a part of the stress-reduction session. The application of correct abdominal massage protocol is a great tool to balance the activity of the autonomic nervous system and decrease the stress level in the client. The author absolutely correct when she stated that the abdominal massage helps the client to reduce “…suppressed emotions” during the therapy.
In the article author gives short description of nine steps abdominal massage which should be incorporated in every massage session. It is short but practically important part of the article which the practitioners can start to use immediately.





Table Lessons. I Am Sorry, Was I Staring? Massage & Bodywork, July-August, pp.84, 2009, by Douglas Nelson
A small but precious article! Bravo! The author described the case of the women he examined. She had several years of intermittent lower back pain, which occasionally radiated down to her leg. His client went through various treatments conducted by a family physician, physical therapist, chiropractor, etc. Everyone targeted her sacroiliac joint and applied treatment did not bring any positive changes. During the examination the author noticed the visual difference in the size of both legs. He correctly concluded that this very simple symptom, which nobody had noticed was, more likely the result of a low grade irritation of the spinal nerve. His client went back to the physician and a MRI of the lower back showed spinal stenosis. His client underwent successful spinal surgery.
The case author described greatly illustrated one important professional requirement for every practitioner who would like to be successful in somatic rehabilitation: “ALWAYS KEEP YOUR EYES OPEN”. Try to notice everything unusual and find a reasonable explanation for it. If you don’t know the answer at the time of the examination or treatment, go to the textbook, use the Internet, ask questions in professional Forums, etc. Never leave the question unanswered for the client and what is more important for yourself.
Another important suggestion is: combine education with trust in yourself and your senses. Everyone can make mistakes and even a medical degree is not a bullet – proof guarantee. This article shows that a skillful practitioner can make a great difference for the client and, furthermore, be very helpful for the physician. According to the article his client’s physician was greatly impressed by the author’s observation skills and knowledge.
The author’s client had the so-called condition of neuropraxia which is chronic low grade irritation of the spinal nerve in the area of the spinal stenosis. At the same degree this condition can affect the peripheral nerve. These cases may develop during the years and the patient may never complain about pain or other uncomfortable sensations in the area of the irritation (lumbar back in this case). Instead the symptoms appear in the parts of the body which are located below the area of original irritation, i.e. in parts of the body where the irritated fibers end to provide innervation of the soft tissue according to the distribution of the nerve. One of the signs of neuropaxia is mild muscle atrophy and weakness. To the author’s credit, he noticed this and made the correct cause-effect correlation.
The only disappointing part of the article is the fact that the author did not try to treat his client. The correct MEDICAL MASSAGE PROTOCOL applied to this client (according to the symptoms he provided in the article) was more than likely able to save her from surgery, but this is topic for another discussion.





Functional Anatomy. Subscapularis. Massage & Bodywork, July-August, pp.87-88, 2009, by Christy Cael
The author tries to keep this section of our Journal alive and well. Again, the article is incorrect.
As in the previous articles the anatomy and biomechanics of the muscle (in this artcile subscapularis) are presented correctly. However the goal of the article is to teach the practitioners how to examine subscapularis muscle using palpation skills and the article is completely incorrect in this instance.
Despite the individual differences in the body’s structure all of us share the same anatomical arrangement. Because of this simple fact medicine has accumulated enough practical knowledge including the correct way of palpation for each muscle. It is really puzzling why the author felt necessity to advocate ways of palpation, which are going against body anatomy and clinical skills.
The somatic rehabilitation, which at this point has more than a century history of successful clinical practice. However this and previous articles leave impression that all authors who greatly contributed, or continue to contribute to the science of somatic rehabilitation, were incorrect in their recommendations.
Let us illustrate this statement. The video below shows the way of the palpation of the subscapularis muscle recommended in the article.
As the reader knows the subscapularis muscle is located on the anterior surface of the scapula, i.e. this muscle is situated between the scapula and ribs. Yes according to the article’s recommendations the practitioner will be able to palpate the subscapularis muscle from this position but it will be only very small part of it. The rest of the muscle is simply unaccessible from this position. Such way of palpation is not clinically informative and it will mislead the practitioner.
Everyone can make mistakes, but three incorrect articles form a pattern. We do not want the readers to think that our reviews are somehow pretentious. For this reason let us open Volume I of Travell and Simmons Myofascial Pain and Dysfunction and see what this milestone of somatic rehabilitation tells us about the palpation of subscapularis muscle. The video below recreates the recommendations from the Travell&Simmon’s work, which is in use by physicians, physical therapists, chiropractors and massage practitioners around the world.
As you may see in the video the correct way for optimal palpation of the subscapularis muscle is completely opposite to the author’s claims. At the same time it is the ONLY clinically informative one.
In the position recommended by the author (on the stomach) the weight of the upper extremity which is dangling from the table and the force of gravity presses the scapula against the posterior surface of the thoracic cage. As result, the subscapularis muscle is also pressed against the ribs and it limits access to the muscle. However, the position of the client on the back as well as the placement of the scapula and the upper extremity off the table (see second video) allows greater access to the subscapularis muscle for the palpation and treatment if it is necessary. In this case the weight of the upper extremity, as well as the force of gravity, work for the practitioner’s benefit. Please compare both approaches and be the final judge.





Essential Skills. Posterior Tibialis Injuries. Massage & Bodywork, July-August, pp. 92-97, 2009, by Ben Benjamin
A very good, informative article which contains a lot of practical information (evaluation, treatment, home exercises, etc.) the practitioners may use immediately.
We would like to add only one more aspect. As a major treatment option for the injured tendon of the posterior tibialis muscle the author correctly recommended the application of friction. However, as a result of tendon injury, the muscle itself will exhibit protective muscle tension and more likely active the trigger point(s). The anatomical location of the tibialis posterior muscle under the gastrocnemius and soleus muscles do not allow direct access to the muscle. This is why the practitioner must add gentle application of postisometric muscle relaxation as a part of the session after the acute symptoms of the inflammation in the tendon subsided.
If there is no tendon injury but there are clinical signs of the muscle strain the same treatment must be added to deep massage on the calf and the exercises recommended in the article. This important addition to the recommended protocol will guarantee stable clinical results.




The Many Faces of Bell’s Palsy. Massage & Bodywork, July-August, pp.99-103, 2009, by Ruth Werner
This is a very informative article which gives good review of the etiology, pathology and clinical picture of the Bell’s Palsy. It looks like the treatment options were not the primary goal of the article. At the very end of the article the author mentioned the massage therapy as a possible method of the therapy.
However, we would like to emphasize that MEDICAL MASSAGE PROTOCOL for Bell’s Palsy is an irreplaceable treatment tool for the patient affected by this disorder. Actually there are four MEDICAL MASSAGE PROTOCOLs which are designed separately for each stage of Bell’s Palsy: acute stage, palsy stage without active movements, palsy stage with weak active movements and residual stage. The best treatment scenario for the patient is involvement of the massage practitioner as soon as possible. In such cases the practitioner who uses the correct MEDICAL MASSAGE PROTOCOL is able to greatly speed up the patient’s recovery using each protocol according to his or her recovery progress.
At the end of this review we would like to say that there is no medication (except the corticosteroids during the initial 2-3 days) or other medical procedure which able to help the patients with Bell’s Palsy. The most common way of treating this abnormality is to wait in hope that facial nerve will recover itself and an application of exercise. The biofeedback and electrical stimulation mentioned in the article mostly used to deal with the residual symptoms. Thus, the MEDICAL MASSAGE PROTOCOL is the ONLY therapeutic modality which works for the patient’s benefits since the first day of Bell’s palsy.



Myofascial Technique. The Temporomandibular Joint. Part I. Massage & Bodywork, July-August, pp.110-115, 2009, by Til Luchau
This is the first part of the article on TMJ dysfunction. The good part of the article is very helpful 3-D illustrations of the anatomy of TMJ and recorded movements of the lower jaw and articular disk.
The examination of the client with TMJ presented in this part of the article is correct, unfortunately is not complete. There are several more tests which are much more informative and helpful for the examination of the TMJ.
Massage Today





Massage and Alzheimer’s Disease. What Would Maslow Say? Massage Today, 9(7):7;16;20, 2009, by Ann Catlin
This is great article and the author did a great job of emphasizing the connection of touch therapy and Alzheimer’s Disease. She is completely correct when she emphasized the importance of touch and sensory stimulation to enhance the life of the person with this debilitating abnormality.
The author made a very powerful correlation of touch therapy for the patients with Alzheimer’s Disease and Maslow’s Theory of humanistic psychology. It strongly speaks about her intellectual potential and make her article even more believable. We now wait for the author’s promised follow up article on the same subject.





Spotlight on Palmaris Longus. Massage Today, 9(7):7;16;20, 2009, by Judith DeLany
This is an important article for the massage practitioners because it discusses the frequently overlooked subject of Dupuytren’s contracture. The author presents the anatomy and physiology of the palmaris longus muscle and its role in developing the tension in the palmar aponeurosis or Dupuytren’s contructurre.
The article doesn’t provide any practical recommendations for the actual treatment protocol for Dupuytren’s contracture. In the article the author suggests the link to the website where the practitioners may find the appropriate treatment protocol. We followed the suggested link and would like to confirm that the advised website contains neuro-muscular therapy protocol for the forearm and hand in a step by step application with informative illustrations to support it.


The Risks of Vascular Compression in Soft-Tissue Therapy. Massage Today, 9(7):8;12, 2009, by Whitney Lowe
The article discusses the risks associated with vascular compressions during massage therapy. We may split the article into two parts: possible compression on the anterior neck and under the occipital ridge.
The first part of the article touches a very important topic of which many practitioners are not aware. We greatly compliment the author for the raising this important topic. He is completely correct when he points out that even gentle massage on the anterior neck may irritate the carotid sinus with a following sudden drop of blood pressure and a decrease of the heart rate. The author also correctly pointed to another even more dangerous outcome of the massage performed on the anterior neck of older clients: embolization of brain by atherosclerotic plaque’s fragments. Even without massage strokes or chiropractic manipulations detachment of the fragments of the atherosclerotic plaque is one of the major causes of the ischemic stroke.
We would like to add our voice to support the author’s pledge for all massage practitioners: Never work on the anterior neck between anterior edge of the sternocleidomastoid muscle and trachea if you did not have a special training and if you work alone in your clinic or in spa setting. Sooner or later you will face the complications of your therapy and it is not in your or your client’s interests.
The second part of the article discusses the risk of compression of the vertebral artery by massage strokes below the occipital ridge which, according to the author, cause the vertebrobasilar insufficiency (VBI) or decrease of the blood flow through the pool of vertebral arteries which supply the posterior part of the brain. The author provided the explanation of his theory and supplied two references from the medical journals, which according to the article supported the potential risk of VBI while the massage strokes are applied below the occipital ridge. This part of the article is completely incorrect and it will keep the practitioners from working in this critically important area. However, for the readers, the claims in the article may sound very well grounded. Considering the possibility of danger to the client, claimed by the article, we would like to explain in detail why practitioners should disregard the second part of this article.
Fig.1. Position of the head and the practitioner’s hand associated with the VBI (according to the article)
In Fig. 1 we recreated, using the picture from the article, the position of the client’s head and the practitioners’ hands. The author states that “…some people could have VBI from techniques such as those (see Fig. 1), with only the weight of the head (underlined by JMS) applying the pressure” and “Problems occur when pressure is applied directly into the occipital tissues”. In such cases the article proclaimed that the practitioner may compress the vertebral arteries and, as a result, the symptoms of VBI will be triggered.
Let us go back to the anatomy textbooks. There are two vertebral arteries which originate from subclavian arteries then, ascending up and on the level of transverse process of C6, enter the vertebral column (see Fig. 2). The uniqueness of the vertebral arteries’ anatomy is that during their further ascending they penetrate the transverse processes of each cervical vertebrae which has a special opening (called transverse foramen) on each side for the right and left artery. Thus, both vertebral arteries pass through the bony canals formed by the transverse processes of C1-C6 vertebrae located on top of each other (see Fig. 2).
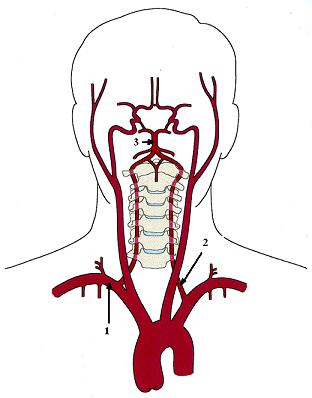
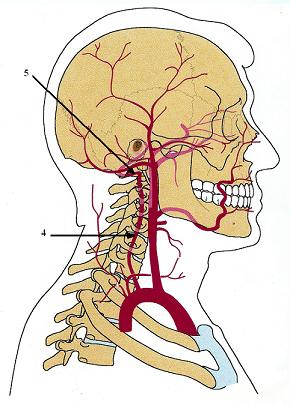
Fig. 2. Anatomy of vertebral arteries
2 – left vertebral artery
3 – basilar artery
4 – right vertebral artery ascends passing through the transverse processes of the cervical vertebrae
5 – vertebral artery point
After each vertebral artery leaves the transverse foramen of the C1 it is located in the suboccipital space between the inferior surface of the skull and upper surface of the C1. This is the area where, according to the article, the application of the massage strokes may cause compression of the vertebral arteries.
So what really happened there? After leaving the transverse foramen of the C1 each vertebral artery makes a small loop and gets into a special depression in the vertebral arch of the C1 called the sulcus of the vertebral artery (see Fig. 3). After passing over the arches of C1, both vertebral arteries unite together to form the basilar artery which supplies the posterior part of the brain (see Fig. 2).
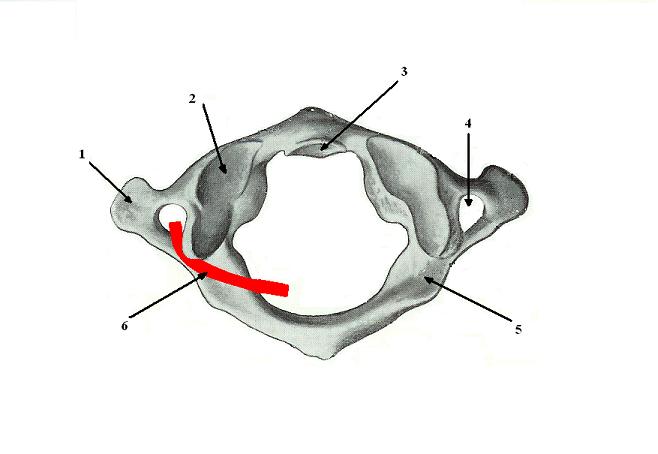
Fig. 3. First cervical vertebra (atlas). Superior view
2 – superior articular process which forms the atlanto-occipital joint with the occipital bone of the skull
3 – articular surface for the C2 vertebra (axis)
4 – transverse foramen in the right process
5 – sulcus for the right vertebral artery
6 – left vertebral artery in the sulcus
Nature recognized the vital role of the vertebral arteries; and this is why both arteries are so well hidden and protected. If massage strokes under the occipital ridge were able to diminish blood flow through the vertebral arteries just from the ‘weight of the client’s head’ or using moderate pressure the human race would have been extinct long ago because of the high vulnerability of the brain’s blood supply.
There is no possible anatomical way to claim that the practitioner may diminish the blood flow through the vertebral arteries while working in the suboccipital area, because he or she does not have any access, pressure wise, to both arteries from this position.
Head extension which is shown on Fig. 4 and mentioned in the article as an additional compressing factor, also does not jeopardizes the vertebral arteries because they are located in the special depression in the arch of C1 (i.e., sulcus) and if there is not a sudden forceful head extension, for example during a car accident, or fracture of the C1, the vertebral arteries will be never in any danger. The hyperextension may cause VBI-like symptoms but they are the result of the increase of the blood perfusion to the brain while the client’s head is placed backward rather than compression of the vertebral arteries. Such compression is usually a result of violent hyperextension as in the result of an accident.
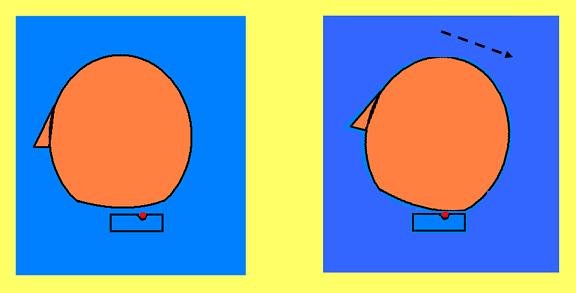
a. Regular head placement b. Head extension
Fig. 4. Head position
Fig. 4 shows the position of the vertebral artery during regular head placement (a) and the head extension (b). The square under the head indicates the lateral view of C1 and the small red circle indicates the cross section of the left vertebral artery located in the sulcus. As you may see, head extension actually protects the vertebral arteries from any application of direct pressure while it eliminates the possibility of the compression of both arteries between the skull and C1. Part ‘b’ of Fig. 4 shows that the head extension brings the occipital ridge and the lamina of the vertebral arch of the C1 close to each other while the left vertebral artery remains out of danger because is safely located in the sulcus.
Overall there is only one small spot where the vertebral artery can be directly accessed by the practitioner. This spot is called the vertebral artery point and it is located on the side of the suboccipital area. This point is used for the treatment of Headaches and/or Essential Hypertension caused by Vertebral Artery Syndrome. Anatomically this area is restricted by the occipital ridge and mastoid process from above and by the transverse process of the C1 vertebra below.
Another risk the article mentions is head rotation which may trigger VBI. The article offers references from medical journals which are supposed to support this idea. To clarify this situation we found both articles to be frank and to be able to have productive intellectual discussion.
In the first article (Dabus, G et al., 2008 click here to read abstract) its authors describe case of VBI after the forceful chiropractic adjustment of the neck. Yes, indeed the forceful adjustment of the neck especially if the soft tissue wasn’t prepared by massage therapy before manipulation may trigger VBI. However, even the authors of the cited article state that it is a very ‘uncommon case’. Finally the authors of this article detected the compression of the vertebral artery between the thyroid cartilage and the transverse process of C6 on the same side and between C1 and C2 on the contralateral side as a result of chiropractic adjustment. Both areas do not have anything in common with the possible compression of the vertebral artery in the suboccipital area claimed by the reviewed article.
Compared to the chiropractic treatment the massage therapy uses different modalities and, as far as we know, the massage practitioners are not trained and never use the adjustments of the neck in their practice. Thus head rotation during regular passive stretching of the neck as well as massage strokes will never trigger VBI.
In the second article (Mitchell, J., et al., 2004 click here to read abstract) its authors examine the clinical validity of the Vertebrobasilar Insufficiency Test as a part of the examination of the patient by chiropractors before the neck adjustment. It is great that the author of the reviewed article informed the readers about the existence of this test and the way of its application. However, the main question remains unanswered: Why are the massage practitioners who never adjust the cervical vertebrae and always work within physiological range of motions should afraid of VBI and stay away from the suboccipital area?
Both articles were written for the chiropractors to inform them about rare but possible complication of the cervical adjustments. This information doesn’t have anything to do with the work all readers of this Journal or Massage Today Journaldo during their practice.
On the contrary, we greatly encourage the practitioners to work in the suboccipital area. It is one of the main clinical tools used to decrease tension in the posterior cervical muscles which insert into the occipital ridge, free the greater occipital nerve and cure chronic headaches. Ironically enough, the massage in the suboccipital area is the first critical step in the application of the MEDICAL MASSAGE PROTOCOL in order to treat the patients with Vertebral Artery Syndrome (VAS). It allows to decrease the tension in the atlanto-occipital joint (i.e. junction between skull and C1) and eliminate chronic irritation of the sympathetic plexus which controls vasoconstriction within poll of the vertebral arteries. VAS may cause chronic headache and what is most important and a little known fact, VAS is one of the leading causes of Essential Hypertension.
VAS is a result of chronic irritation of the sympathetic nervous plexus which control vasocnstriction/vasodilation of the vertebral arteries. The reason for this irritation is tension of the posterior cervical muscles (which by the way insert into the occipital ridge) which is directly responsible for the misalignment of cervical vertebrae. As a result of this misalignment both arteries slightly twist while they are ascending through the cervical vertebrae and this fact triggers VAS. Thus, VAS is never considered a result of compression of the vertebral arteries in the suboccipital space.
As a conclusion, please pay great attention to the first part of the article andcompletely disregard its second part which is based on groundless fear, and it ties-up the practitioners’ hands, diminishing the effectiveness of the treatment of many important pathological conditions.





Deadbeat Diagnosis: “Chasing the Pain” Massage Today, 9(8):1; 7; 16, 2009, by Erik Dalton, PhD
What can we say? This is an excellent article! It is very well written, greatly illustrated, has important practical value for the practitioners, based on the science and it stimulates the readers’ clinical thinking.
The article is not written in the so called ‘journalistic style’ which frequently allows the authors to hide their inability or unwillingness to write a professionally important piece. Neither has it the promotional component in it. This is exactly how articles in the professional journals must look like. Thank you!





Trigger Point and Treatment of the Serratus Posterior Superior. Massage Today, 9(8):1; 7; 16, 2009, by David Kent
This good and informative article on the serratus posterior superior muscle (SPSM), its examination and treatment. The practitioners {do not} encounter the hypertonic muscle abnormalities in SPSM in everyday practice. The active trigger points there will develop in cases of long, chronic muscle tension on the upper back. Usually, these clients have much more problems with active trigger points in the trapezius, levator scapulae and rhomboid muscles. In the majority of cases the successful treatment of hypertonic abnormalities in these muscles will take care of the active trigger points in the SPSM. Thus, the practitioner rarely sees the isolated case of active trigger point in SPSM.
The author is completely correct when he says that clients with the chronic pulmonary disorders will exhibit active trigger points in the SPSM. However, even in these cases other muscles on the upper back we mentioned above will exhibit hypertonic muscle abnormalities and formulate leading clinical symptoms.
The final comment we would like to make is to regard to the treatment. We would like to specially emphasize the fact that the trigger point therapy alone does not have enough clinical power to completely eliminate the active trigger point, especially in the deeply located muscles like SPSM. The practitioner needs to address the soft tissue in the area of active trigger point on a layer – by – layer basis to completely eliminate even residual symptoms of the tension in the fascia or at the insertion of the soft tissue into the bone structures.
Massage Therapy Journal





Body Mechanics for Stretching. Massage Therapy Journal, 48(2):105-108, 2009, by Dr. J. Muscolino
The subject of correct body mechanics for the massage practitioners is one of the major professional issue which stays under the radar. The body mechanics look like a very simple matter. However, in real life it is one of the major problems for the massage therapy profession. Incorrect body mechanics ruins the practitioner’s body, makes him or her easily exhausted, and restricts the technical potential because many sophisticated massage techniques are impossible to execute without correct body mechanics. Very frequently, readers telling us that they prefer Shiatsu or Lomi-Lomi to the Swedish massage because kneading and other techniques hurt their hands. The only answer to such letters is to change or learn correct body mechanics. In such case you will work with your body instead of your hands.
The major blame is incorrect education in the massage therapy schools. As soon as the practitioners learn body mechanics incorrectly or more frequently don’t learn it at all and develop their own incorrect way it is very difficult to break the wrongly established pattern.
This is why this article is a rare piece which addresses at least part of the issue: correct body mechanics during stretching. Of course, the author was able to formulate only the basic concept and illustrate it on several examples, but even such short articles on this subject are rare and welcome events.




Fighting Fibromyalgia Pain. What Research Says About Using Massage Therapy To Help Ease the Pain of Fibromyalgia. Massage Therapy Journal, 48(2):101-103, 2009, by B. Menard, PhD and C. Piltch, PhD
This is another article which discusses the important subject of Fibromyalgia (FM) and the role of massage therapy in the treatment of clients who suffer from this abnormality. The authors are correct that there is controversial information from the scientific sources if massage therapy indeed helps patients with FM. This inconsistency is the result of an absence in the united view on what should be done and what should be avoided during the treatment. Until the basic concept of medical massage is established and recommended to the practitioners we will encounter the same problem over and over again.
Despite the fact that the authors mentioned the fact of a decrease of ATP production in the skeletal muscles affected by FM they sided with the commonly accepted theory of FM development as a result of decrease in serotonin production in the brain. Of course, it may be their personal belief, but to be completely frank with the readers they should at least mentioned the fact that there is another theory which sees FM as failure of mitochondrias in the affected muscles to produce the necessary amount of ATP. In such cases the changes in serotonin and substance P are results of the chronic pain stimuli constantly bombarding the central nervous system. This theory is of great importance for the massage practitioners because it explains why the correct protocol of massage therapy shows great clinical results for patients with FM.




Dealing With Diabetes. Massage Therapy Journal, 48(2):36-42, 2009, by J. Milivojevic
The author deserves professional appreciation for bringing up the subject of diabetes treatment using massage therapy. Her article is based on personal stories of success, but she also relied on the recommendations of Dr. T. Field, the Director of Touch Research Institute. Her advice on applied pressure, and techniques can be used by practitioners immediately to help clients or loved ones who suffer from diabetes.
We would like to support the article and add that the regular massage sessions are a vital therapy for the clients with diabetes. Of course, the massage therapy is not a silver bullet, but it is a great treatment tool to prevent further complications (edema, angiopathy, neuropathy, etc.) The correctly presented educational brochure on therapeutic impact of massage therapy on diabetes (this article can be used as template) will assist the clients to better understand the goals of the treatment and it will help the practitioners to build up their practice.
Massage





Life Support. How Touch Therapies Promote Fertility. Massage, 158, Jul-Aug, 62-67, 2009, by Phyllis Hanlon
A very important article! The author provides a general overview of the role massage therapy plays in the treatment of infertility and briefly describes several clinics where training and treatment is offered.
This part of massage therapy has a very limited professional exposure because of laws and regulations prohibiting massage practitioners working on any inner parts of the body. However it can be done in the clinic under medical supervision.
The basic concept of Gynecological Massage (GM) was developed in1868 in Sweden by T. Brandt. His initial goal was to develop treatment which will be able to assist women with infertility problems. It combined external and internal work. GM is a first treatment option which is recommended to the patients in many European fertility clinics.
This article is important because it gives the practitioners another window of opportunity to expand their practice and helps women with low cost, effective therapy to promote their fertility.

Release Restrictions With Visceral Manipulations. Massage, 158, Jul-Aug, 56-61, 2009, by Dr. Jean-Pierre Barral
Visceral massage is a critically important part of treatment of inner organ abnormalities and it also enhances somatic rehabilitation. Dr. J-P Barral is a very well known author and his work deserves great professional respect. This is why this article is so disappointing. Overall it is a promotional piece which provides little practical help or theoretical education for the practitioners. What may readers learn from the article?:
1. Visceral manipulations are important and should be used by the practitioners
2. Fascia and inner organs are interconnected
3. A long description of author’s career, achievements and studies he participated in without the actual outcomes of these studies
4. The only practical recommendation in the article is: “Therapists will let their hand glide over the client’s body with a pressure equal to the weight of their hand. The hand is found to be attracted (how exactly? JMS) toward the restricted areas (i.e., inner organs)”
This is a very strange practical recommendation. Let us say, as an example, that the practitioner stands facing the client along the right side of the table and he or she follows the article’s recommendation to simply slide the hand along the abdomen from lower parts of it to the epigastric area in hope that affected inner organ will some magical way attract the hand. In described case the right or left hand (depends which one the practitioner uses) will have tendency to go to the left side of the abdomen (or to the right of the practitioner) simply because the practitioner’s body position and body mechanics. The practitioner will be mislead by this fact alone and may declare to the client, for example, that he has problems with the descending colon. Considering the fact that the article doesn’t have any other practical recommendations this single suggestion, without any theoretical or practical information to back up the article’s claims, sounds very strange indeed.
Another important fact we would like to mention. According to the basic concept of the visceral massage, this treatment must be conducted by the specially trained massage practitioner only after the diagnosis was established by the physician (gastroenterologist, hepatologist, urologists, etc.). We have never read in either medical or massage literature that the massage practitioner should conduct visceral manipulations on the client using his professional diagnostic skills alone as a justification of such therapy.
For example, any visceral manipulation in the left abdominal flank is strictly forbidden, if the patient has Ulcerative Colitis. However, if the practitioner is not familiar with this and other important precautions he or she may put the client’s health at great risk. This is why the decision to use any visceral manipulations on the clients with the abnormalities in the abdominal cavity must be coordinated with the client’s physician first. We would like to remind the readers that the author of the reviewed article is a physician himself and he has all the rights and abilities to operate independently for his patients’ benefits. However, the massage practitioner must coordinate his or her therapy with the client’s physician.
We understand that Massage Journal may offer the author limited space for the article. However the author has enough expertise to contribute more to the massage practitioners’ education and practice by building their theoretical or clinical knowledge. Unfortunately both components are missing in an almost four (!) pages article.


Expert Advice. “How Can I Prepare to Work With a Person Who Has Cancer or a History of Cancer?” Massage, 158, Jul-Aug, 50-53, 2009, by Tracy Walton
Overall this is a good article which raises awareness about the role of massage therapy in the treatment of the cancer patients and emphasized its importance. These days the practitioners may rely on multiple medical publications which confirmed the increase of the concentration of the T- and B-lymphocytes, which are responsible for the cellular and humoral immunity, in the patients with cancer who underwent the course of massage therapy.
However, there is one aspect in the article which is controversial and the author makes claims which do not have any medical sense. The author firmly states that massage therapy does not have ANY contraindications for the patients with acute cancer. She did not back up these claims with any medical sources and we have a real problem with that. The number one rule of medicine formulated long ago by Hippocrates is “Do not harm!”
The author sees concerns about the application of massage therapy during the acute cancer stage as a myth. In such case we have a legitimate question to ask: Can the author personally guarantee to every patient with acute cancer that her recommendations will never facilitate the spread of metastasises?
If the author is not able to provide this personal guarantee that in 100% of cases her recommendations will never jeopardize the patient’s health and massage practitioners who will follow these recommendations will never work against the patient’s health she doesn’t have any right as a health practitioner to publish this statement. If the author takes such 100% personal responsibility it means that she looks on a very complicated pathological condition superficially and this is a great mistake which put the client’s health at risk.
The author stated that the increase in the blood circulation as a result of massage isn’t a factor in the possible cancer spread and the article correctly pointed out that the increased circulation as a result of exercise is not considered as a compromising factor.
Let us quote the article: ‘In fact, the more we have learned about cancer spread, the less it is attributed to the simple mechanical movement of cancer cells through the blood. Instead, as several authors have pointed out, metastasis is a function of more complex physiological and chemical factors’
We demand the medical sources, which clearly state that modern oncology doesn’t recognize anymore the role of mechanical factor in the movement of the cancer cells through the lymph and blood circulation.
Even from the quote above it is obvious that the author has omissions in her views. First of all, physiological factors can’t play role in the cancer development because the word’physiological’ means a normal body function. No one can describe cancer from the physiological point of view but rather the ‘pathological’ or ‘pathophysiological’.
Other part of the quote is much more troubling. The cancer may spread via blood (hematogenous way) or via lymph circulation. The spread of the cancer via blood circulation (mentioned in the quote) is usually associated with a very aggressive types of cancer or with long cancer history and unsuccessful therapy. Cancer must invade the blood vessel to use hematogenous way of spread. The blood vessels are much more resistant to the cancer invasion compared to lymphatic vessels because the last ones do not have the basement membrane. This is why “The invasive tumor cells may penetrate the lymphatic channels more readily than blood vessels” (E. Rubin, H. Reisner: Essential of Pathology 5th Edition, 2008).
This is a critical point where the article unintentionally misleads the practitioners. The fact of increased blood circulation during massage treatment in acute stage is not a real fear, but increase of the lymph circulation which the author did not mentioned at all is.
If the cancer has already sent metastasis via blood application of massage it doesn’t make any impact on the client’s health because metastasis has already landed somewhere. However, if the cancer spreads by the lymphatic system which is more frequent, the increase of the hydrostatic pressure within lymph nodes by massage strokes during acute stage is contraindicated. For the client’s health benefits his matter should not be even discussed the way as it is presented in the reviewed article. Of course the formation and spread of metastasises from the area affected by the cancer is much more complicated process that just mechanical movement of the cancer cells, but this factor plays the leading role in the cancer spread.
Let’s take as an example the patient who has a rectal cancer. The lymph drainage from the rectum partly drains into the inguinal lymph nodes. The same packs of lymph nodes will receive the lymph from the lower extremities. Let’s us quote the basic medical anatomy textbook (April, 1990):
‘Because the lymph vessels of the rectum parallel the arteries, metastatic carcinoma of the rectum may disseminated widely within the abdomen, pelvis andinguinal nodes (underlined by JMS)’.
According to the basic concept of the article, massage of the lower extremities in the acute stage of the rectal cancer is supposed to bring health benefits for the patients. This is not exactly the case. In the majority of patients, the rectal cancer develops silently and when he or she starts to look for the help frequently the lymph nodes already invaded. From the moment the rectal cancer was diagnosed the patient is considered to be in the acute stage. His or her massage practitioner, following the article’s recommendation, will suggest to use intense massage therapy to stimulate immune system. The practitioner will work on the both lower extremities with the same massage protocol as on the upper extremities. As a result the practitioner will stimulate the lymph drainage from the both lower extremities and this fact alone will greatly increase the hydrostatic pressure inside of the inguinal lymph nodes which may already host cancer cells. These lymph nodes are the first line of the body’s defense against cancer. In the lymph nodes the cancer cells are under attack by immune system and this process takes time. Excessive increase of hydrostatic pressure inside the lymph nodes by massage strokes on the lower extremities, while lymph nodes are dealing with cancer cells, will empty them earlier when the job is not done. This factor alone may play a role in the further spread of the cancer cells to the next pack of lymph nodes.
As soon as the cancer is removed and the patient goes through the chemo- and radiation therapy or he/she in the remission the author’s recommendations to fully engage the entire client’s body in the course of massage therapy is correct. However during the acute stage the practitioner may use massage therapy as a treatment option only if he or she has the clear understanding where the cancer is located and how lymph drainage to and from this area is functioning to avoid increase of the hydrostatic pressure inside of the lymphatic system below the area affected by the cancer.
Thus, the article has incorrectly generalized recommendations to every cancer patients instead of educating the readers on the correct application of the massage therapy for the cancer patients keeping in mind their interests first. We would like to repeat one more time: ‘Do not harm!’
Category: Good Apples, Bad Apples
