The purpose of this section of the Journal of Massage Science to inform the practitioners about valuable articles that frequently go unnoticed, as well as to point to those authors and publications who exhibit low educational standards. We do not play politics and we are not associated with any publishing company or professional association. We are a completely independent voice and we promise you direct unbiased reviews based strictly on the science.
If the author of the reviewed article does not agree with our opinion, we will be more than happy to publish his or her response and have a productive discussion over the article’s subject.
At the end of the year we will recognize and reward the author of the most important publication(s) and point to the authors of the most unscientific publication(s). We hope this will help to raise the bar of published materials in massage journals for the benefit of the entire profession.
Our Editorial Board would like to introduce the Appreciation Award for the American massage publication which has contributed the most important articles to the science of massage therapy in 2009.
The trophy is made from polished brass on a marble pedestal with an exotic wood foundation and decorated with blue agate. Its dimensions: 10 x 8.8 x 8.8″ (25 x 22 x 22 cm).

The symbolism of the Appreciation Award: letter M indicates massage; the two serpents represent twin roles – preventive and medical – of massage; two serpents form the heart which represents love and compassion of our wonderful profession.
Our Editorial Board will present the Appreciation Award at the beginning of 2010.
Massage Today




Massage and Alzheimer’s Disease. Part 2. Massage Today, 9(9):14, 2009, by Ann Catlin, LMT, OTR
This is Part 2 of the article written by Ann Catlin. We are in complete agreement with the author that massage therapy is an important treatment tool for patients with Alzheimer’s Disease. These patients will receive great benefits from the incorporation of regular massage therapy sessions into their well being.
Another important aspect of this article is the encouragement to massage practitioners to contact the facilities and members of the patients’ families and offer their services. The research information in the article is based on the latest scientific publications in several medical journals (Dementia; Geriatric and Aging, American Journal of Geriatric Psychiatry) and it supports the idea of using massage as an important treatment tool for patients with Alzheimer’s Disease.
The article gives the practitioners enough scientifically based leverage to talk with the management of the live-in facilities and members of the families to explain benefits of the therapy. Working with these patients and seeing their progress is professionally rewarding, but it also will generate an additional source of income for the massage practitioners to help them to survive and prosper in difficult economic times.




Your Clients With Lyme Disease. Massage Today, October: p.16, 2009, by Ruth Werner, LMT
A very good and informative article on Lyme Disease, its origin and symptoms associated with this pathological abnormality. However, the article gives very little information on massage treatment options for these patients. At the same time the patients with Lyme Disease will get significant benefits from the regular application of massage therapy because the soft tissue and joints of these patients are greatly affected. Of course, massage therapy is not a critical factor in the treatment of Lyme Disease, but it greatly reduces the intensity of the somatic symptoms and helps patients recover more quickly.
The basic rules of engagement are the application of the regular massage strokes in the direction of the lymph drainage, with intensity of the strokes below the pain threshold mostly concentrating on the affected areas. Use of gentle local stretching and passive stretching during the client’s prolonged exhalation is part of this treatment as well. It seems a very simple protocol, but the regular application of the massage therapy really makes a huge difference for patients with Lyme Disease.





Red, White and Black Reaction. Massage Today, October: p.14, 2009, by Leon Chaitow, ND, DO
An excellent article! As usual Dr. Chaitow brings up a very important subject. The clinical importance of the white or red dermographism reaction is mostly unknown to massage therapists and Dr. Chaitow’s article brings it to the practitioners’ attention. The article gives a general description of the subject and we would like to say that so far this article is the single source for this information which is recently published in massage journals.



Thumb Pain and Brachialis Muscle. Massage Today, October: p.1; 12, 2009, by David Kent, LMT, NCTMB
The subject of the article is referred pain in the thumb as a result of the tension in the brachialis muscle and consequent entrapment of the sensory branch of the radial nerve on the arm. The entire article heavily relies on Travel and Simmons “Trigger Point Manual”.
The author is correct in that the tension in the brachialis muscle may indeed entrap the sensory branch of the radial nerve and cause the referred pain to the thumb. However, there are several aspects which greatly decrease the value of the article.
First of all the article gives the impression that the irritation of the sensory branch of the radial nerve by the brachialis muscle alone is a commonly occurring problem. In fact, it is a very rare abnormality and the brachialis muscle is not the first major factor which contributes to the referred pain to the thumb. In fact, it is quite the opposite. The low – grade irritation of the brachial plexus on the anterior neck (by the anterior scalene muscle) or on the anterior shoulder (by the pectoralis minor muscle) are the most common reasons for the referred pain to the thumb which is also called Radial Nerve Neuralgia.
If the brachial plexus is irritated on the anterior neck or on the anterior shoulder the patient first of all will feel sensory abnormalities in the most distant parts innervated by the affected nerve(s).
Let’s hypothetically assume that the brachial plexus is irritated by the anterior scalene and/or pectoralis minor muscle for two to three weeks. As a result of low – grade irritation of the brachial plexus, muscles of the arm, forearm and hand will exhibit active and sleeping trigger points. If the part of the brachial plexus which gives origin to the musculocutaneous nerve is affected the brachialis muscle will always harbor active trigger point(s) because this nerve innervates the brachialis muscle. As a result of active trigger point and tension, the brachialis muscle loses its softness and now it may entrap the sensory branch of the radial nerve with following radiation of pain to the thumb. In this case in order to eliminate pain in the area of the thumb the practitioner must free the brachial plexus first, and only after that address the brachialis muscle itself.
The scenario we described above is much more common in every day practice than the chance of having isolated trigger point in the brachialis muscle only.
Is there a chance that the brachialis muscle alone will harbor the active trigger point(s) and entrap the sensory branch of the radial nerve? Yes, there is such a chance, but it is only in a very tiny minority of the patients with Radial Nerve Neuralgia. The brachialis muscle is a synergist (or helper) to the biceps brachii muscle which is a very powerful prime mover. The patient must completely exhaust the prime mover first to exhaust the muscle synergist (i.e., brachialis). The article correctly mentioned one category of the patients: violin and viola players who practice for hours using the same repetitive movements. However even in these clients the tension in the anterior scalene and pectoralis minor muscles must be ruled out first.
Another potential group is the patients who had ruptured or detached biceps brachii muscle but surgery wasn’t performed on these patients in order to restore the function of the damaged muscle. In these cases, the brachialis muscle becomes the prime mover and this fact alone may be responsible for the symptoms of the Radial Nerve Neuralgia. As you may see, the Radial Nerve Neuralgia, as a result of the tension in the brachialis muscle, is a very rare abnormality. Of course, it is great that the article exposed the practitioners to this rare abnormality. However, our concern addresses the fact that other much more clinically important causes of the referred pain to the thumb weren’t even mentioned in the article.
The information we just reviewed addresses the first part of the article which describes the anatomy of the brachialis muscle and pathophysiology of the trigger points developed there. This part of the article relies solely on Travell and Simmons publication. This book originally was written for physicians because it doesn’t offer any massage therapy protocols for the treatment of hypertonic muscular abnormalities and concentrates on the stretching, injections and muscle energy techniques. To fill this gap many massage educators developed their own massage therapy protocols using the textbook’s diagnostic palpation techniques as a guidance for the therapy. Unfortunately, it does not always work and this is exactly what happened to the second part of the article which proposes massage treatment for the brachialis muscle.
The article suggests a five step protocol, which is supposed to release pressure in the brachialis muscle. We have real problem with Steps 3-5. The practitioner who follows these recommendations may very easily hurt the client and make the clinical picture worse because this treatment is based on incorrect anatomical and clinical data.
The brachialis muscle has a very complicated anatomy in regard to the major nerves and vessels of the arm and the proposed treatment has a great chance of irritating these structures.
Let’s look on the anatomy of the area discussed in the article. Fig. 1 shows lateral view of the pathway of the radial nerve on the upper extremity.
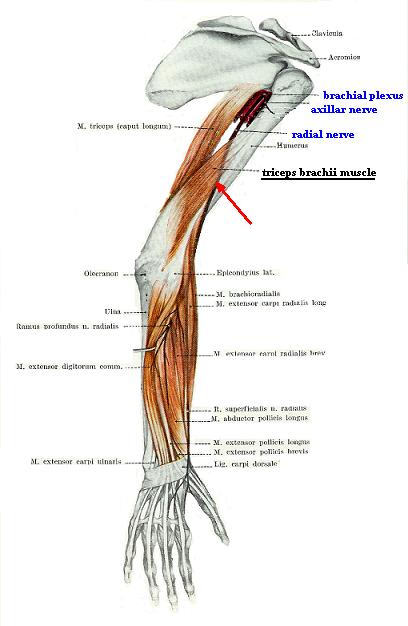
Fig. 1. Pathway of the radial nerve on the upper extremity
As you can see the radial nerve originates from the brachial plexus shown in the arm pit in this view, starts to go down on the medial surface of the arm and after this wraps around the shaft of the humerus and on the border between the lower and middle thirds of the humerus (under the triceps brachii muscle) it appears on the lateral surface of the arm. While following this complicated route the radial nerve remains very close to the bone shaft, especially on the lateral surface of the humerus.
Nature recognized the danger of radial nerve location, because it can be very easily compressed against the bone by traumatic force or simply by the powerful triceps brachii muscle. To avoid that the shaft of the humerus in this area has a special depression called sulcus of the radial nerve where this nerve safely located. In other words the radial nerve lies on the bone itself. In Fig. 1, this area is emphasized by the red arrow.
The video below re-creates Step 3 as it is recommended in the article. You may notice that the practitioner moves the biceps brachii muscle medially first to expose the brachialis muscle under it and apply gliding strokes at a 45 degreesangle (pay attention to the position of the thumb).
Let’s come back to the original topic of the article. The tense brachialis muscle compresses the sensory branch of the radial nerve and it causes referred pain to the thumb. Great! The article correctly established the cause and effect sequence. In such case we may be 100% sure that radial nerve is inflamed because of its irritation by the brachial muscle. Now, we would like readers to fully understand the traumatic impact of the suggested strokes when the practitioners must “apply treatment at a 45 degrees angle against (bold by JMS) the humerus” gliding along the lateral edge of brachialis muscle. This recommendation will additionally traumatize the already inflamed radial nerve through compressing and rubbing the sensitive nerve tissue against the solid bone (see red arrow in Fig. 1). How on earth is it supposed to decrease inflammation in the nerve?
The video below re-creates Step 4 from the same protocol. Now, you may now see that the practitioner moves the biceps brachii muscle laterally and applies the same strokes against the humerus along the medial edge of the brachialis muscle.
This part of the treatment is even stranger. Fig. 2 (a) shows the anatomy of the medial surface of the arm. As the reader may see the median and musculocutaneous nerve (which innervate the brachialis muscle) as well as the brachial artery are located exactly long the medial edge of the brachialis muscle. In such case, the article recommends compressing the major nerves and artery of the upper extremity against the bone (i.e. humerus) along they pathway on the medial surface of the arm. The black arrow in Fig. 2(b) indicates the direction of the massage strokes suggested in the article. Please note that the strokes go over the exact pathway of the major artery and nerves on the medial surface of the forearm.
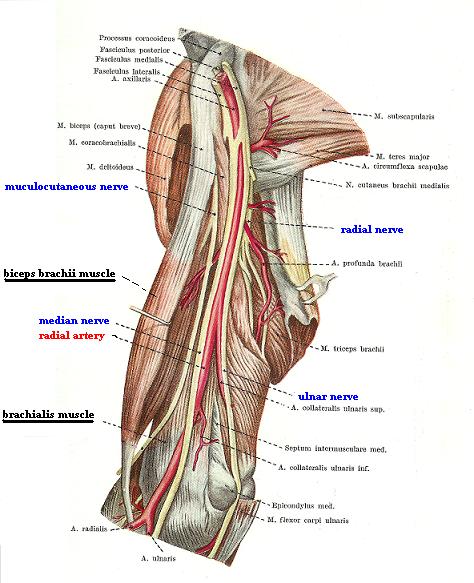
a
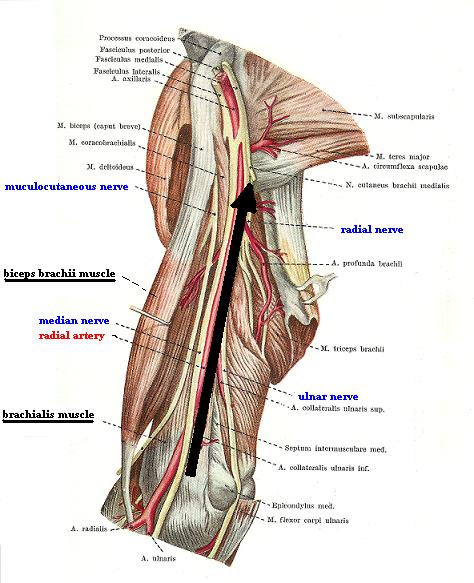
b
Fig. 2. Medial surface of the arm (biceps brachii muscle is pulled laterally)
Yes, there are cases in medical massage therapy (tension in the brachialis muscle is not one of them) when the practitioner needs to work along the major nerves and artery in this area. However he or she should NEVER direct massage strokes compressing tissue with major nerves and artery against the bone at a 45 degrees angle! They must be directed only superficially along the drainage. The recommendation in the article is just plain wrong and it does not have anything to do with the science of somatic rehabilitation.
The video below re-creates Step 5 from the same protocol. It seems that excessive rubbing and compression of the major nerves on the arm separately on lateral and medial surfaces of the arm wasn’t enough. Now the practitioners must apply bi-manual compression against the bone along both edges of the brachialis muscle at the same killing 45 degrees angle and slide upward additionally irritating the major nerves on both surfaces of the arm at the same time.
The video below shows the correct way to address the brachialis muscle. Of course, medical massage treatment of the tension in the brachialis muscle is much more complex, however, the idea of this video is to correct the information published in the article.
The first part of the video shows the application of similar gliding strokes on the lateral surface of the arm. There are two major differences when compared to the treatment recommended in the article (Step 3):
1. The article did not mention the necessity of forming a fold of the skin before mobilization of the biceps brachial muscle in the medial direction. Lack of this important part greatly increases the tension in the soft tissue and builds up pressure on the radial nerve even before treatment begins. The correct procedure is shown in the beginning of the video.
2. It is completely wrong to advocate treatment when the pressure against the humerus must be applied under a 45 degree angle. The video shows that the thumb must glide forward horizontally and the pressure must be directed, not against the humerus but just slightly above. In such cases, the practitioner glides along the actual edge of the brachialis muscle without compressing the already inflamed radial nerve against the humerus.
It is forbidden by human anatomy and basic clinical science to apply pressure against the humerus on the medial surface of the arm under the biceps brachii muscle using a 45 degree angle. Thus, the practitioner never accesses the brachialis muscle from the medial surface. This is not supposed to be even a matter of discussion in any article on massage therapy.
Instead, the practitioner should apply special kneading techniques on the biceps brachii muscle. This allows him or her to knead the brachialis muscle against the ANTERIOR surface of the humerus using the biceps brachii muscle as a clinical tool. The final part of the video shows this treatment. The black arrow in Fig. 2(b) indicates the direction of the massage strokes suggested in the article. Please note that the strokes go over the exact pathway of the major artery and nerves on the medial surface of the forearm.
We are not giving any final comments because we would like the readers to make their own professional decision in regard to the clinical validity of this protocol basing it on information we provided as well as on their personal knowledge and experience and just plain common sense.
Massage Therapy Journal




Nurturing Touch. MTJ, 48(3): 42-47, 2009, by Clare La Plante
The article raises the very important issue of autism and how massage therapy may help children with this abnormality, also their parents. As several research studies have pointed out and furthermore based on our and other practitioners personal experience massage therapy is an essential component for the treatment of a child with autism.
Treatment for autism, including the application of massage therapy, is a very complex topic which deserves special discussion, but we would like to emphasize one important issue. The child with autism especially a very young child is isolated and lives in, as one author correctly called it, an ’emotional cocoon’ when he or she has difficulties in communicating with the outside world, and even parents. When a child with autism gets older and parents are persistent with their attempts to fight disease, he or she improves communication skills and overall it frequently improves the autism. However, for the parents, the management of young children and attempts to break this cocoon become a major problem.This is where massage therapy is a great help.
The article correctly outlines massage therapy benefits for the children and mentions involvement of the parents. However, the issue is much more complex. For young children with autism the connection with the outside world must start with the creation and strengthening of the bond with their parents. This is a unique, first step for the successful management of autism for the rest of the patient’s life. The earlier this process is started the better chance for the child’s recovery. However in many cases this important time is missed because it is a very difficult to get through to young children with autism.
This is why the regular massage therapy conducted by parents is so important. The best help the massage practitioner can do for the children with autism is to train the parents first and let them work on the child on a daily – or every other day – basis. Only after two to three months of such treatment the practitioner should consider his or her involvement if inflamed parents have decided to consult him or her. For older children the treatment can be started by the practitioner, but the parents must be present, at least at the beginning.
The author of the reviewed article cited the results of the study conducted by Touch Research Institute in Florida. In the study she described a similar protocol was used. The scientists from the Touch Research Institute understood the importance of the enforcement of the child-parent bond for the successful treatment of autism. This is why the Institue trained parents and let them conduct the massage treatments on the children enrolled in the study. Dr. T. Field and her colleagues then used various tests to examine the impact of massage therapy on the children with autism assigned to both the clinical and control groups.
Massage





Research. Massage 160, Sept.: 96-99, 2009, by Editorial
Massage Journal published abstracts of two studies which examined the effect of massage therapy and they were conducted in Japan and Turkey. The publication of results of research studies like these definitely benefits the entire massage therapy profession because they equip the practitioners with enough scientific information to educate other health practitioners and clients on the importance of massage therapy.
The first study (Kohichi Takamoto, et al., Journal of Physiological Studies, Feb, 2009) showed how the application of trigger point therapy greatly helps the patients with pain and fatigue. The interesting aspect of the study is the fact that the authors showed that trigger point therapy, besides the reducing local tension in the muscles, is able to balance the activity of the autonomic nervous system by decreasing the tone of its sympathetic division and increasing the parasympathetic tone. This study, as do many studies before supports the idea of reflex mechanism of massage therapy as one of the leading factors in the healing process.
The second study (Gamze Ekici, et al., Manipulative and Physiological Therapeutics, Feb. 2009) concentrated on the very important topic of the treatment of Fibromyalgia using massage therapy. The authors compared the results of the application of manual lymph drainage massage and connective tissue massage on the intensity of the pain in the Fibromyalgia patients. Patients from both groups showed sufficient decrease of pain intensity, but the patients from the group treated with lymph drainage massage showed slightly better results.
We greatly appreciate the efforts of the Massage Journal to keep the practitioners informed about new scientific developments in the field of massage therapy.




Create Balance with Reflexology. Massage 160, Sept.: 78-84, 2009, by Michele Milder
The article is a general review of Reflexology, its history, healing mechanisms and place of this type of bodywork in the modern school of somatic rehabilitation. The article is written on behalf of the Reflexology Association of America, and it can be helpful for those practitioners or newly graduated massage practitioners who are in the process of making decision about new modalities they would like to learn in order to extend their practice. This article will greatly serve these individuals.





Lymph Formation. Massage Therapy’s Effect on the Lymphatic System.Massage 160, Sept.: 66-70, 2009, by Joachim E. Zuther
This is a very good article on the function of the lymphatic system and lymph formation. It is especially helpful to those who have just considered learning the lymph drainage massage and implement it into their practice.
The article provides a very short only four paragraph review of massage impact on the lymphatic system, but apparently it was not the main subject of the article. Thus from the point of basic science it is a very informative article.




Stay the Course. 3 Keys to Injury Prevention and Career Longevity.Massage 161, Oct.: 60-64, 2009, by Marc Westergard
A very good and needed article. It does not have the goal of providing comprehensive information on body mechanics but it accomplishes a lot. In simple language it emphasizes the importance of using the practitioner’s body weight as a structural component of the massage strokes and give the practitioners basic guidelines on how to prevent injuries and unload thumbs during the treatment.





Deep-Tissue Massage Made Easy. Massage 161, Oct.: 40-46, 2009, by Marc Westergard
Same massage publication, same issue and same topic as an article written by Mr. M. Westergard but what a difference! There are a lot of issues in the article which are wrong. To save time we sent readers the article on Body Mechanics in the current issue of our Journal. Here we will concentrate only on one issue: ‘No-Thumb Zone’.
We are all professionals here and before we start we would like to ask our readers one hypothetical question. Would you pay for the deep tissue massage while on vacation or in the local spa if you will know ahead that practitioner who will work on you uses only various compressions, gliding strokes with fists, knuckles and forearms? If you answered ‘yes’ to this question skip this review. If you, as a client, are not happy with such an approach to your massage session we would like to save you and your practice from the information in this article and what is more important from the potential enrollment into the seminar on the same subject.
Dear readers, welcome to a new breakthrough in the massage science: ‘No-Thumb Zone’! We are not kidding. This is how one of paragraphs in the article starts: “I often inform therapists they have entered into the no-thumb zone when they attend my workshops”.
We may compare each massage session with solo performance of a talented violinist. Would you listen to the violinist who does not use his or her thumbs? The article simply cuts off great massage techniques from the arsenal of practitioner. There is no place for the friction or kneading in ‘no-thumb zone’. For us it feels like professional helplessness.
The article correctly mentions that thumbs are the major areas of stress on the practitioner’s hands during the massage session, but the offered solution is simply stunning. We think that instead of spreading bizarre ideas of no-thumb massage which destroys the soul of massage therapy the article should concentrate on the science of using correct body mechanics to unload the hands and thumbs during massage session. It should emphasize necessity of extensive arsenal of basic massage techniques which allows the practitioner to constantly alternate their application to engage other parts of the hands. It should teach the massage practitioners to take care about their hands and thumbs before and after the session and after the work day. Instead we have ‘no-thumb zone’!
Several members of our Editorial Board are in the private massage practice and they as well as our students are able to conduct many sessions per day without stressing their hands and thumbs. When the practitioner is equipped with enough knowledge based on science, he or she is able to easily enjoy work while delivering unforgettable experience to the clients. We think that ‘no thumb’ approach is not a productive way to build up massage practice especially in these economic times. It is a professional dead end!
Massage & Bodywork





Myofascial Techniques. The Temporomandibular Joint. Part 2. Massage & Bodywork, Sept-Oct 120-125, 2009, by Til Luchau
This is an excellent article! The article concentrates on only one part of the TMJ treatment: tension in the digastric muscle. The successful treatment of TMJ dysfunction requires the work on all major players (temporalis, masseter, etc.) and several articles published recently in the massage journals provided this information. However the role of the digastric muscle in the TMJ dysfunction is rarely even mentioned. The article made a great contribution, emphasizing the importance of the treatment of digastric muscle used to reverse TMJ dysfunction. The 3-D informative illustrations are of great help.




Essential Skills. Anterior Tibialis Injuries. Massage & Bodywork, Sept-Oct, 102-107, 2009, by Ben Benjamin
This is a good article! It gives all the information the practitioner needs (from anatomy to treatment and home exercise program) in order to address the injuries of the tibialis anterior muscle.
We have only one small addition to this article. The article suggests that cross fiber friction should be used on the inflamed tendon of the tibialis anterior muscle, this is a correct recommendation. However, the article also states that: “After using the friction therapy to break down some of the scar tissue, massage the foot, calf and shin to enhance circulation into the tendon”
From the optimal clinical effectiveness, the treatment should be conducted in the opposite sequence: foot, calf, shin, and only after that work on the tendon itself. In such case the practitioner releases tension and protective muscle spasm in all soft tissue of the foot and leg first to make the friction treatment more clinically effective in regard to fighting with the inflamation in the tendon itself.
In the case of tendinitis in any location the treatment must also include a very careful passive stretch of the affected muscle or careful application of the muscle energy techniques, especially Postisometric Muscular Relaxation. In this case the friction becomes much more effective because the tibialis anterior muscle is relaxed, and it does not elicit additional tension on its tendinous part.





Functional Anatomy. Quadratus Lumborum Muscle. Massage & Bodywork, Sept-Oct 97-98, 2009, by Christy Cael
Another article – another mistake! All articles by the same author published during this year are united by similar mistakes. The purpose of these articles is to teach the massage practitioners to palpate muscles. This is a noble goal because this information is rarely addressed. The problem with all of the articles published so far is the fact that they recommend the palpation of the middle layer of the skeletal muscles through the fibers of the superficially located muscles. This is a waste of time and efforts because if the muscle in the middle layer harbors the active trigger point(s) the superficial muscle located on top of it will always exhibit protective tension which will ruin the palpatory efforts of the practitioner to examine the muscle located in the middle layer. At the same time there are ways of the palpation which the practitioner should know and use in order to examine the muscles in the middle layer to have direct access to them.
These techniques are essential diagnostic skills and seems that neither article even mentioned their existence. We showed the correct application of these techniques in the previous issues of the Journal of Massage Science.
Let’s look at where this article went wrong. To support our review we will use Travel and Simmons ‘Trigger Point Manual’. This is not the only source of the palpatory examination but it is the most respected and frequently cited publication on somatic rehabilitation. In the video below we recreated, for the readers, the palpatory examination of the quadratus lumborum muscle from the article.
There is no clinical way the practitioner is able to reach and examine the quadratus lumborum muscle from this position. If it harbors the active trigger point or hypertonus the lumbar erector will immediately exhibit protective muscle tension and examination becomes useless. The approach you see in the video allows the practitioner to examine the belly and lateral edge of lumbar erectors.
In the video below we re-created the correct palpatory examination of the quadratus lumborum muscle from the Travel and Simmons’ textbook. If you compare both videos you may clearly see the huge difference in the approach.
In the video the dotted line indicates the spinous processes of the lumbar vertebrae, the waved lines indicate the medial (letter ‘M’) and lateral (letter ‘L’) edges of the lumbar erectors, the solid lines indicate the lower edge of the 12th rib and iliac crest and the dashed line indicates the lateral edge of the quadratus lumborum muscle.
Notice the difference in the location of the thumb while the practitioner examines the lumbar erectors, than its lateral edge and finally the lateral edge of quadratus lumborum muscle.
The correct way of palpation allows the practitioner to examine the fibers of the quadratus lumborum muscle directly. Thus, the way of palpation advocated in the article is used only for the examination of the lumbar erectors and it is completely useless for the examination of the quadratus lumborum muscle.





Table Lessions. Wait Don’t Hang Up. Massage & Bodywork, Sept-Oct: 94, 2009, by Douglas Nelson
We really enjoyed articles written by Mr. D. Nelson. They are case studies, written in the easy, informative way frequently with a hint of humor and they are what massage therapy is all about. Frequently the massage therapy becomes the last helpful tool which solves the patient’s health issues quickly and efficiently. We can’t agree more with the author when he states that clinical effectiveness of the massage practitioner relies on three crucial skills: ‘… listen carefully to all details, hear what the client describes as connected, and know the literature’. We may add only one more aspect, to actively ask questions to confirm details and find out previous clinical symptoms the client didn’t mentioned because he or she didn’t think they are connected to the current problem(s).
C-K Andrade, P. Clifford.
“Wolters Kluwer/Lippincott Williams&Wilkins”, 2008
ISBN-13: 978-0-7817-6760-6
Recently our Journal was asked to review the Second Edition of a textbook called Outcome-Based Massage. Usually we don’t review books and we didn’t plan to change our policy. However after reading even small sections from different chapters we realized that we hold a gem of a publication in our hands.
The textbook takes the students and practitioners from the very first steps of massage therapy science to the application of different medical massage modalities (neuromuscular therapy, connective tissue massage, lymph drainage massage, etc., etc.) for the somatic rehabilitation. Even rarely mentioned in massage literature percussion massage to enhance the bronchial drainage in cases of chronic pulmonary abnormalities is in the book. Each chapter has proper references and every section has great educational and practical value.
The great strengths of this textbook lies in its attention to detail and the dedication of the authors in building up the practitioners’ clinical thinking. We can rave about the value of the textbook for several pages but we think that it is simply better for the readers to get this publication and we are sure it won’t disappoint you.
We think that the authors made only one mistake. The title of the textbook does not reflect its value and frankly one may pass the textbook in the catalog just because of that. This, of course, is our personal opinion.
Category: Good Apples, Bad Apples
