The purpose of this section of the Journal of Massage Science is to inform the practitioners about valuable articles that frequently go unnoticed, as well as to point to those authors and publications who present very questionable views in their writings. We do not play politics and we are not associated with any publishing company or professional association. We are a completely independent voice and we promise you direct unbiased reviews based strictly on the science.
If the author of the reviewed article does not agree with our opinion, we will be more than happy to publish his or her response and have a productive discussion over the article’s subject.
At the end of the year we will recognize and reward the author of the most important publication(s) and point to the authors of the most unscientific publication(s). We hope this will help to raise the bar of published materials in massage journals for the benefit of the entire profession.
Massage Today
Massage & Bodywork Magazine
Massage Therapy Journal
Massage Magazine
Massage Today





Massage Therapy Reduces Pain for Patients in a Postoperative Thoracic Surgery Care Setting. Massage Today January, 2012, Vol. 12, Issue 01, by Massage Therapy Foundation Contributor
A very important article that informs readers on the results of a clinical study conducted at The Mayo Clinic in Rochester, Minnesota. The study examined the efficacy of massage on postoperative patients after thoracic surgeries. The original article was published in International Journal of Therapeutic Massage and Bodywork. The results of the study confirm the clinical value of massage therapy in pain control and quicker recovery in patients after thoracic surgeries. Practitioners may use the results of this study to establish referral relationships with local thoracic surgeons.





A Golfer’s Worst Nightmare Rehabilitated Through Massage. Massage Today January, 2012, Vol. 12, Issue 01, by Debbie Roberts, LMT
An excellent article! In a short format without any unnecessary information, the author was able to clearly explain to the reader the mechanisms of potential injuries associated with golf based on her own client-illustrated clinical assessment.





Freeing the Heart. Massage Today January, 2012, Vol. 12, Issue 01, by Dale G. Alexander, LMT, MA, PhD
Rarely, is the topic of this article mentioned in massage literature. There are large numbers of educators, books, DVDs, etc., some correct and some without any merit, that try to educate therapists on how to address active trigger points, help clients with Carpal Tunnel, etc. There is minimal exposure of practitioners to the idea of using therapeutic or, in better cases, MEDICAL MASSAGE PROTOCOLs for clients with inner-organ disorders. However, there is a large body of scientific data in existence that such MEDICAL MASSAGE PROTOCOLs have been developed and are successfully practiced. The article summarizes the author’s personal experience in addressing the function of the heart through various types of chest compression and massage.
In clinical reality, MEDICAL MASSAGE PROTOCOLs are more complicated than this basic concept but the author deserves considerable credit for determining some basic principles on his own and using them on his clients. We would like to express our own opinion that successful clinical use of MEDICAL MASSAGE PROTOCOLs for patients with inner-organ abnormalities under the control of a physician is one of the highest proficiencies in the massage therapy profession.




Practice Building with Postural Analysis. Massage Today January, 2012, Vol. 12, Issue 01, by David Kent, LMT, NCTMB
This article emphasizes the importance of postural analysis and sharing this information with the client before and during the treatment course. Such approach will definitely help build trust and confidence in the client, and give the practitioner hints if he or she is selecting the correct treatment protocol. We may disagree with the title of the article since actual clinical results are what build a successful practice.




Giving a Big Thumbs Up for the Healthy Thumbs. Massage Today February, 2012, Vol. 12, Issue 02, by Judith DeLany, LMT
An excellent and informative article that teaches practitioners about the importance of the thumb, its anatomy and biomechanics. The article also contains information on preventive measures to keep the thumb functionally healthy.
Concerning possible abnormalities associated with the thumb, the article mentions the so-called skier’s thumb. Despite the presence of this abnormality, Periostitis of the 1st metacarpal bone along the insertion of abductor policis brevis muscle and De Quervain’s disease are the most common abnormalities associated with massage therapy but unfortunately they were not mentioned.





A Massage Protocol for Peripheral Neuropathy. Massage Today February, 2012, Vol. 12, Issue 02, by Rita Woods, LMT
This is the second part of an article that presents massage protocol for diabetic peripheral neuropathy. It seems that the main component of the protocol, after proper preparation, is necessity of “working the tissue to the bone” or, in other words, is to increase pressure to the deepest level. The article based this approach on the belief that such treatment will increase circulation and help the nerves recover since diabetic neuropathy is a direct outcome of circulatory abnormalities.
The author is completely correct by linking diabetic neuropathy with circulatory abnormalities but she completely misunderstood the nature of this process. The circulatory abnormalities cause pathological changes in the peripheral receptors and, ultimately, in the nerve trunk and to the same degree affect the circulation in the soft tissue. The main outcome of this process is extreme fragility of the capillaries and larger vessels and vulnerability of the soft tissue to any typeof excesses. This why the first recommendation an endocrinologist will offer every patient with diabetes is to take care of the feet: avoid injury, tight shoes, dry skin, lower temperatures, infections and so on. This article is the first time in any source we have read that a massage therapist must use pressure “to the bone” as a clinical tool to help clients with diabetic neuropathy. The practitioner should stimulate local circulation in a client with diabetic neuropathy using fast, repetitive strokes in the direction of drainage rather than deep pressure. The disadvantage of using deep pressure is damage to already vulnerable lymphatic vessels and additional obstruction of the lymph drainage. This is such a harmful recommendation and goes against the most basic clinical common sense.
For this review, we analyzed almost 50 medical sources around the world that examined the effects of various bodywork modalities used on patients with diabetes. The studies were done in the United States, Italy, Spain, Russia, China, Iran, etc. and published in the medical journals that range from Evidence Based Complement Alternative Medicine to Diabetes and Diabetes Care. This is what we found as treatment modalities: Swedish Massage, Connective Tissue Massage, combination of massage and exercise, Lymph Drainage Massage, Reiki, Underwater Massage, Acupoint Massage.
As readers will notice, all these modalities have one thing in common-they use light to moderate pressure. This article in Massage Today is the only one that recommends “to the bone” pressure for patients with peripheral neuropathy without any statistically backed analysis and solely based on R. Woods’ controversial ideas, which do not contain scientific proof nor make any sense.
Instead of recommending senselessly pressing into tissue, the article should recommend stimulation of local circulation with fast, effleurage strokes in the direction of drainage using extra oil, applying electric vibration along the anatomical pathways of the peripheral nerves, stretching peripheral nerves to decrease pressure build up in the epineurium, etc. All these components are lacking in the article, yet mindlessly applying pressure to the bone is recommended. This article illustrates the fact that the author does not understand the complex mechanisms behind diabetic neuropathy.
There are a couple of other genuine surprises in the article. The author recommended the same protocol for the treatment of clients with chemotherapy-induced peripheral neuropathy. However, in these cases the peripheral neuropathy has a completely different mechanism. It has nothing to do with impaired circulation but rather with toxicity of the medication used during chemotherapy. If circulatory problems are secondary to the dying peripheral receptors, the application of deep pressure on the client with chemotherapy-induced peripheral neuropathy is simply professional incompetence. Rather than use such an extremely painful treatment on a person who already has gone through physical and emotional pain and suffering because of cancer, various sensory stimulations of the affected areas-light vibration, percussion, pinching, ice/cold application, etc.-should be substituted.
Finally, the article stated that a therapist must check the client’s feet because “gas gangrene first appears as a tiny dark spot.” Where did this come from? First of all, gas gangrene appears as an area of hyperemia and without emergency surgical intervention, gangrene will kill the patient in 24-48 hours. Patients with diabetes have a chance of developing “dry gangrene,” which has nothing to do with “gas gangrene.” How can someone write an article on diabetes and not bother to check such basic information about diabetes? Google would be great starting point.
Dry gangrene is the result of impaired circulation while gas gangrene is outcome of a highly virulent infection. Many practitioners today work with physicians frequently in their office. It is difficult to imagine how any physician will not become panicked after a massage practitioner, who after reading this article inMassage Today, states that he or she suspects gas gangrene in the patient. Such an assessment will forever discredit the practitioner in the eyes of the physician.
Clostridium perfringens, which causes gas gangrene, is such a virulent bacteria that the operation room is closed for a complete and very meticulous cleanup following any surgery for gas gangrene. Is there someone on the Massage Today Editorial Board who is supposed to check articles before their publication to avoid such embarrassing blunders and misleading pieces?
Pagano L, Proietto M, Biondi R. Diabetic peripheral neuropathy: reflections and drug-rehabilitative treatment. Recenti Prog Med., 2009 Jul-Aug;100(7-8):337-42.

Freeing the Heart. Massage Today February, 2012, Vol. 12, Issue 02, by Dale G. Alexander, LMT, MA, PhD
The “inside-out” technique discussed in this article is much less effective than the application of combined Thoracic and Abdominal Pump Techniques if one intends to normalize pressure in the thoracic cavity.
What is really puzzling is how the article tries to explain the mechanisms associated with the effectiveness of the “inside-out” technique:
“…the downward and medial stretch gaps the loose connective tissues allowing the thoracic pressure to flow from an area of greater concentration to one with a lower concentration.”
Thoracic pressure does not flow. The pressure is not a liquid to flow and has fluctuations in concentration. The intrapleural pressure remains always negative. There is alveolar pressure, which fluctuates during inhalation/exhalation, and there is transpulmonary pressure that is always positive.
Tension in the diaphragm makes it flatter and, as a result, intrapeural pressure becomes less negative. The patient feels it as shallow and frequent breathing. Additionally, the negative intarpelural pressure is a major driving force of the venous blood flowing into the right heart. No one would like to equalizepressure in the thoracic and abdominal cavities. In fact, it is to the benefit of the patient’s health to maintain the difference because less negative intrapleural pressure means more trouble for the pulmonary system and cardiac function. In such case, the “inside-out “technique, which as claimed in the article equalizes the difference in pressure between the thoracic and abdominal cavities or in other words will make intrapleural pressure even less negative, will increase pathological symptoms.
So what may contribute to the outcomes of the “inside-out” technique promoted in the article? Based on the description of this technique in the article, it is obvious that it does exactly the opposite. It maintains or enforces the difference between intarpeural and abdominal pressure by decreasing tension in the diaphragm and restores its dome-like shape.





Positional Release Self Care for Soreness and Other Pains. Massage TodayFebruary, 2012, Vol. 12, Issue 02, by Leon Chaitow, N.D., D.O.
What is unique about Dr. Chaitow’s articles compared to the majority of publications we read in massage magazines is the combination of flawlessness and topic that no one else touches. This article is an excellent example of this. In a short, the author efficiently discusses a very important subject of home recommendations used to deal with next-day soreness following massage therapy that each client must obtain from the practitioner before the client leaves therapy room. We cannot stress enough the importance of correct recommendations for the client, his or her confidence in the therapist and the overall impact of homework on the entire treatment strategy. A very important read for anyone who practices or would like to practice the medical aspects of massage therapy.





Hip and Thigh Pain: The Tensor Fascia Latae Connection. Massage TodayFebruary, 2012, Vol. 12, Issue 02, by David Kent, LMT, NCTMB
A very good article on lateral hip and thigh pain. Despite discussing tensor fasciae latae muscle as a major source of pain in these areas, the article also emphasizes the importance of evaluating other potential factors that may trigger a similar clinical picture.





Dealing with Fibromyalgia. Massage Today February, 2012, Vol. 12, Issue 02, by Stuart Taws
This is a great article because it addresses the “sacred cow” subject of the magic map of tender points proposed by the American College of Rheumatology to finalize the diagnosis of Fibromyalgia. Instead of using this map as a supportive diagnostic evaluation, the majority of health practitioners rely on this map as a major diagnostic criteria. The author is completely correct when he states that these points are generally more sensitive in everyone including completely healthy individuals. Now patients are labeled with a “newly established” diagnosis of Fibromyalgia that in many cases is treated as psychological disorder.
As the article correctly pointed out, this “diagnostic tool” becomes a major disaster for many patients with Chronic Pain Syndrome. Thus, when working on the client with Fibromyalgia, be careful to avoid the same trap as other health practitioners before you. In many cases, the Fibromyalgia case you are dealing with is much easier to fix because it is a case of Myofascial Pain Syndrome which was not initially treated right.




Freeing the Heart, Part III: Elongating the Esophagus. Massage TodayFebruary, 2012, Vol. 12, Issue 02, by Dale G. Alexander, LMT, MA, PhD
This is the third part of the article. The first part was very good, the second had some questionable points but third one is a complete disaster. The information in Part III is completely incorrect and exaggerated. The overall topic of Part III is how to free the heart by releasing tension in the esophagus. The article contains so much misinformation that we will only concentrate on the most outrageous.
1. In the article reader will find this passage:
“Common sense suggests that the sac around the heart cringes in its attempt to prevent the acid (from the stomach, by JMS) from penetrating its protective sheathing. In addition, should the acid reach the fibers of the heart muscle, it creates an irritable reaction within them. Might this relate to a host of the different heart ailments that increasingly are described both in abnormalities of electrical transmission within the heart and the increasing frequency of atrial fibrillation?”
Common sense does not suggest this nonsense, and what the author wrote will make anyone with even a basic knowledge of anatomy and physiology speechless. It is the first time in the history of medicine that someone suggested that acid from the stomach might penetrate walls of stomach, walls of pericardium or sac around heart (as stated in this article) and enter the cardiac muscle itself interfering with electrical transmission in the heart and cause atrial fibrillation. It seems that the author sees gastric contents as sulfuric acid that burns through living tissue. Why did the author stopped at heart? If he continues this train of thought, we may expect that gastric acid will continue to burn into the lung, the fascia and eventually will pour through the patient’s skin. This is so wrong and it is even humorous to read such “gem” in the national publication in the 21st century. The only explanation we have is the fact that the author believes that the word “heartburn” actually means that acid burns the cardiac muscle. “Heartburn” is a figurative description of gastric content entering the esophagus as a result of high acid concentration or weakness of the sphincter, which separates the esophagus from the stomach or a combination of both factors. The article is simply sad.
2. Let’s look further. Here is another discovery:
“It is my clinical experience that the SCMs (sternocleidomastoid muscles by JMS) function as guard dogs in preserving the cranium’s safety in the event of a sudden shift in position of the head as may happen in a fall, the body flung forward or backward (bicycle or motorcycle accident) or impact trauma of all kinds.”
It seems that the author has the wrong clinical experience. Readers are professionals and many work on the clients after whiplash injuries. Let ask ourselves a simple question: “What parts of the neck are painful in the client after frontal impact whip-lash injuries?” The answer will be the posterior neck because anterior part of the head is heavier, and when during the collision the head suddenly goes forward it is the posterior cervical muscles that stabilize it to prevent fracture of the cervical vertebrae and spinal cord trauma (Hedenstierna et al, 2009). Yes, the SCMs may be damaged but mostly during a rear-end impact. However, as it was convincingly shown by Elliot et al., (2010) with the use of MRI imaging, the SCMs are not the first to be damaged during an anterior whip lash injury but the longus capitis muscle and longus colli muscle are damaged first and mostly to the degree of fatty tissue proliferation after their trauma. In such cases, SCMs are not the ‘universal guard dogs’ as suggested in the article even within the same anterior cervical group. This is why the author’s clinical experience betrayed him again.
3. This part of the article is ‘pure enjoyment’:
“A unilaterally contracted SCM or bilaterally so, compresses the jugular foramen through which both the vagus nerves and the accessory nerves exit from the brain.”
“…let’s remember that the accessory nerve innervates the trapezius muscles as well as the SCMs. Thus, tight traps are also a tip off that compression of the jugular foramen is a variable and that a contracted esophagus may be a crucial variable flying under the radar as a soft tissue structure that we need to treat.”
We will discuss here the most unbelievable chain of logic we ever read. Let us condense the article’s content: tensed SCM compressed jugular foramen on the bottom of the skull and via this opening vagus and accessory nerve leave the skull – accessory nerve innervates trapezius and SCM muscle – tension in the trapezius muscle is a sign that the accessory and vagus nerves are compressed by SCM in the jugular foramen – vagus innervates the esophagus and its compression causes esophageal shortening – short esophagus puts pressure on the posterior heart limiting its function – proposed treatments, which includes various techniques on the chest and work under the occipital ridge, reduce tension in the trapezius muscle and thoracic cage and it elongates the esophagus.
Great! Everything seems logical plus the article offers a list of references, which, unfortunately, do not support this logical chain but does inject some scientific component in it. Let us look on this seemingly logical chain from the perspective of medicine rather than the author’s personal clinical experience that, as this article shows, undermines his educational contributions.
Let us agree from the beginning that even if one link in the offered chain of events is incorrect the entire logical chain constructed by the author will collapse. In such case, the SCM muscle is unable to compress the jugular foramen, as stated in the article, and as a result irritates the vagus and accessory nerve for one simple reason: it is not even in the vicinity of jugular foramen.
Let us look at Fig. 1 that shows the anatomy of lateral neck with the SCM clearly visible. As we know, the SCM on the skull originates from the mastoid process that is a prominent bone just below and behind the ear. It later goes down and inserts into the clavicle and sternum.
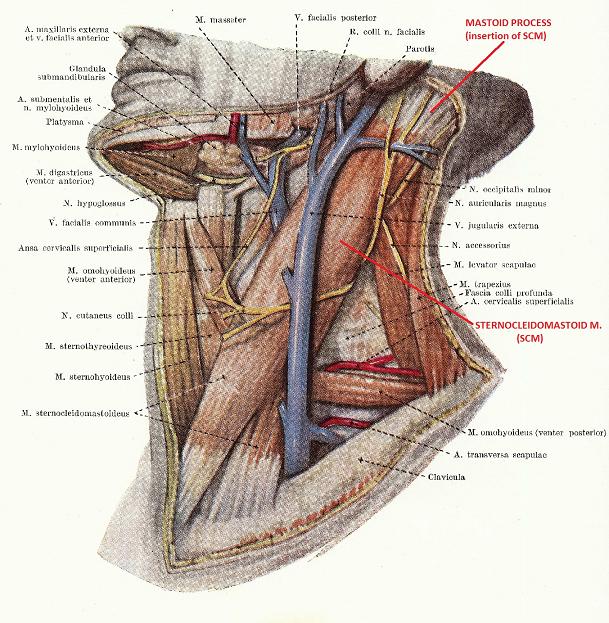
Fig. 1. Superficial lateral neck
Fig. 2 shows the same lateral neck with the SCM muscle cut so the middle layer of the neck is exposed. You may see a small part of the accessory nerve, which is now visible while the vagus nerve is completely absent in this picture.
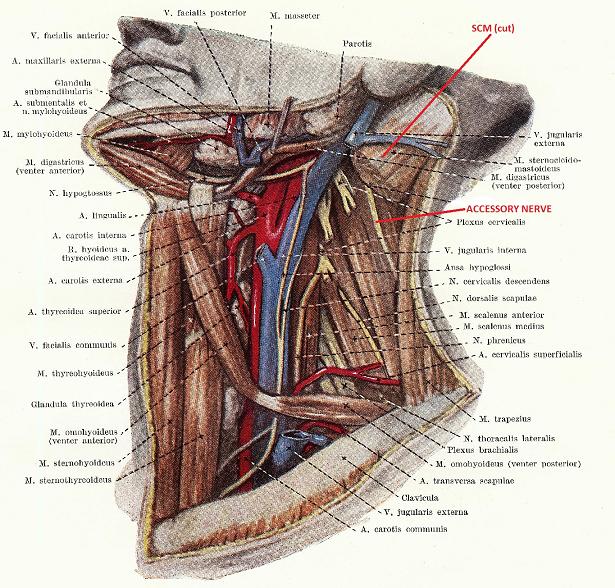
Fig. 2. Middle layer of the lateral neck
Fig 3 shows the anatomy of the deepest layers of the lateral neck where the accessory and vagus nerves are clearly visible just after they left the jugular foramen. As you may see, the jugular foramen, vagus and accessory nerves are located far medially to the SCM.
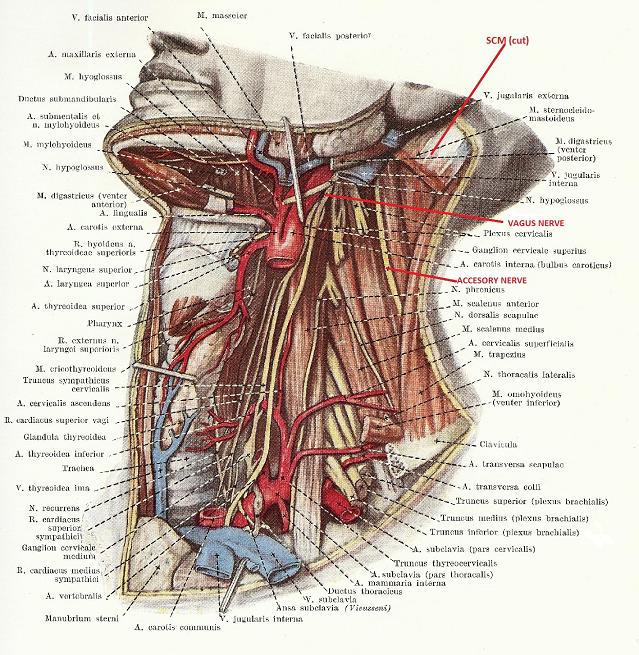
Fig. 3. Deep layer of lateral neck
To shows the actual distance between the jugular foramen and mastoid process where SCM s originated we refer readers to Fig. 4.
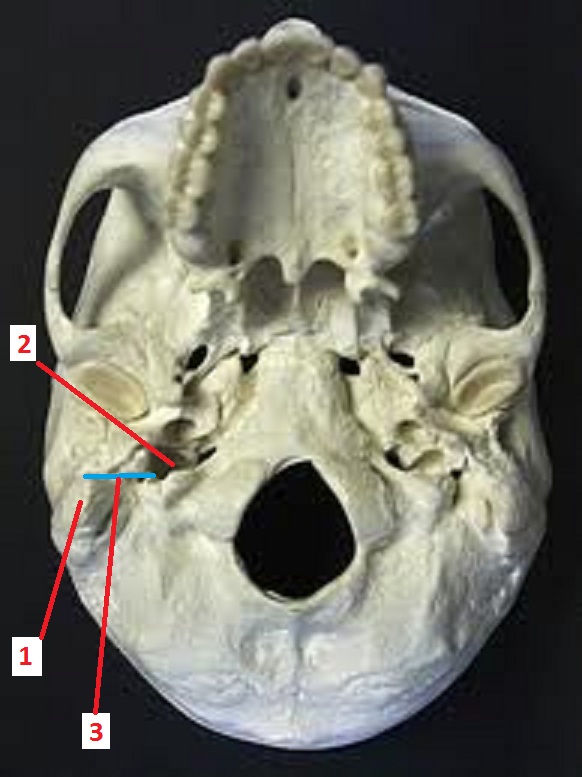
Fig. 4. Deep layer of lateral neck
1 – mastoid process where SCM is originated
2 – jugular foramen
3 – distance between mastoid process in jugular foramen
Fig. 4 shows the bottom of the skull where all openings are clearly visible. Please note the distance between the mastoid process, which is the area where the SCM originates, and the jugular foramen where both nerves exit the skull and, according to the article, the SCM will compress them in the jugular foramen. In real life, the distance between the mastoid process and jugular foramen is approximately 1-1.5 inches depending on the size of the skull.
As you may see in Fig. 4, the SCM is not even close to the jugular foramen and is unable to compress neither the accessory nor vagus nerves. In such cases, there is no justification for the esophagus shortening that the author presents as a cause of cardiac abnormalities. Furthermore, working on the trapezius muscle will not elongate the esophagus. All of this is completely erroneous.
Massage Today is fortunate that cardiologists and gastroenterologists are not readers of this publication, otherwise the editorial board will receive considerable feedback for this article. This article is a prime example of a very common phenomenon in massage publications in which authors twist science in the hope of justifying their very questionable and frequently incorrect views. We are sure that when authors publish their articles in national massage media they must feel privileged and must respect readers by double-checking their data before submitting any article.
Elliott JM, O’Leary S, Sterling M, Hendrikz , Pedler A, Jull G. Magnetic resonance imaging findings of fatty infiltrate in the cervical flexors in chronic whiplash. Spine, (Phila Pa 1976). 2010 Jan 28.
Hedenstierna S, Halldin P, Siegmund GP. Neck muscle load distribution in lateral, frontal, and rear-end impacts: a three-dimensional finite element analysis.Spine, (Phila Pa 1976). 2009 Nov 15;34 (24):2626-33.




Massage Therapy and Joint Mobilization. Massage Today March, 2012, Vol. 12, Issue 03, by Joseph E. Muscolino, DC
This is an excellent and informative article. The author states that:
“This is why chiropractors and massage therapists so often work together. Marrying joint adjustments with massage soft tissue manipulation ideally complement each other ….”
There is nothing more to add. Unfortunately, not all chiropractors share this wise position. Some do not offer massage therapy at all and some rent rooms to massage practitioners as a source of revenue. The majority of those who work with massage therapists send the patients to practitioners after the chiropractic adjustments and it greatly decreases the effectiveness of the “marriage” correctly mentioned by Dr. Muscolino.





A New Method for Dealing with Hip Rotators. Massage Today March, 2012, Vol. 12, Issue 03, by Shari Auth, MA, Lac., LMT, NCBTMB
We faithfully follow publications about Auth’s Method and have reviewed all of them in previous issues of JMS many times. Here is new piece that again advocates using only the elbow and forearm as a therapeutic tool to reduce tension, in this case in hip rotators. There is nothing wrong with the use of the elbow and forearm but what is completely erroneous is when this technique is presented as a “New” method and is the “Only” treatment tool to be used.
Tomorrow someone else will single out, let us say, percussion from the entire arsenal of massage techniques, call it a “New” method and publish articles and conduct seminars based on the idea that percussion should be the only basis for massage therapy sessions.
Recently, the author moved her great new discovery from the field of therapeutic massage to the field of medical or clinical massage. Now she proposes the Auth’s method for various medical conditions in this article on tensed hip rotators. In the pictures that illustrate the article, the confident practitioner is shown happily sticking an elbow in the gluteal area exactly where the sciatic nerve is located, and the author does not even bother to mention the fact that the therapist must be extremely careful in this particular area. Of course, the author did not even consider to mention the fact that tension in the hip rotators very frequently is caused by tension in the L5-S1 segment where treatment needs to concentrate.
The author deserves a lot of credit for her methodical approach to disseminating misleading information. Her articles basically proliferate in massage publications, and it is now Massage Today‘s turn. This is our favorite quote from the article that explains everything about Auth’s Method and the author.
“Left-brain knowledge crammed in during massage school all to be forgotten later, with the exception of the fashionable piriformis.”
In other words, the author suggests professional illiteracy and proudly informs readers about her own. According to the article, left-brain knowledge that schools tried to deliver to the author, is now already forgotten. Furthermore, she assumes that it is forgotten also by all practitioners including readers of Massage Today and this publication. It seems that the author treats her colleagues as grossly incompetent.
According to the author, the piriformis muscle is considered “fashionable.” If author studied properly at school, she may remember that the piriformis muscle is not just “fashionable” but it is the key to the lower extremity. Apparently however, this left-brain knowledge has already left the mind of the creator of Auth’s Method.
It is really puzzling to find Dr. Muscolino and S. Auth’s articles not only under the roof of the same publication, but in the same issue. Does not the Editorial Board of Massage Today realize that by publishing such condescending nonsense it undermines self-education and damages the reputation this publication has worked so hard to developed and maintain?
Massage & Bodywork Magazine





Thoracic Outlet Syndrome (not!). Massage & Bodywork January/February, 33-35, 2012, by Douglass Nelson
This is a very good article that illustrates the importance of clinical thinking. Unfortunately, clinical thinking is underrepresented in massage schools and basically practitioners are left alone to develop it. The article is very helpful in this sense.





Arthritis In Its Many Forms. When To Use Massage and When To Avoid.Massage & Bodywork January/February, 38-41, 2012, by Ruth Werner
A very good article on arthritis, its causes and pathology. The massage as treatment option also is discussed with correct suggestions for its basic rules of application. It is especially important because sometimes it is recommended that Lymph Drainage Massage should be applied to the inflamed joint itself and even such mild application may trigger additional flare up if client has acute Rheumatoid Arthritis. The only thing we would like to add is that Periostal Massage is designed especially for cases of Osteoarthritis and is an extremely powerful clinical tool.




Maintain Strength With a Neutral Wrist Position. Massage & BodyworkJanuary/February, 43-45, 2012, by Barb Frye
The article reminds practitioners of the importance of maintaining the wrist in a neutral position during application of various massage strokes to avoid injuries. We cannot agree more. Thank you for the reminder.





Functional Anatomy. Latissimus Dorsi. Massage & Bodywork, January/February, 47-48, 2012, by Cristy Cael
Correctly presented anatomy, function and palpation skills for the latissimus dorsi muscle. The client’s stretching at home is also helpful information.




Diabetes and Massage: Translating the Evidence. Massage & BodyworkJanuary/February, 50-55, 2012, by Diana L. Thompson
The article is a very good overview of scientific data on diabetes and its basic management including massage therapy. It helps readers understand the complexity of the problem and provides considerable helpful recommendations to clients, friends and members of the client’s family.





Bodyreading the Meridians. The Spiral Line. Massage & BodyworkJanuary/February, 94-99, 2012, by Thomas Myers
As usual, an excellent article by T. Myers. There is nothing to add, and we recommend it to our readers.





Fretting Over Musician’s Injuries. Massage & Bodywork January/February, 100-105, 2012, by Whitney Lowe
An excellent, clinically oriented article! It addresses a very rarely mentioned topic, somatic abnormalities correlated with a particular profession. In this case, the article discusses injuries and tensions that musicians may sustain as a result of repetitive movements. We highly recommend this article to readers and keep in mind the information from the article when they have a new client who is musician.




Quadriceps Injuries. Massage & Bodywork January/February, 106-111, 2012, by Ben E. Benjamin
A very good and informative article on quadriceps injuries, diagnostic tests, treatment options and the client’s home-exercise program. In regard to treatment options, Friction Therapy is mostly mentioned. We would like to add that if active trigger points are present, Trigger Point Therapy, and Postisometric Muscular Relaxation are two critically important tools that need to be combined with Friction Therapy.




Working With Rib Restrictions. Massage & Bodywork January/February, 112-115, 2012, by Til Luchau
An excellent, informative article with very helpful illustrations. There are a couple of things we would like to add. In the examination part of the article, it states that the practitioner must examine each rib separately to find out if the client had restriction in the costovetebral joints. For this purpose, it is recommended that vertical pressure be applied to each rib.
“Each rib should give slightly if you put anterior pressure on it”
This recommended test is very helpful indeed but the degree each rib “gives” under direct-pressure application mostly comes from the costal cartilage at the insertion of each rib into the sternum. The natural process of aging accompanies the normal decrease of elasticity of cartilaginous part of each rib. Thus, the practitioner who uses this recommended test as guidance to the therapy must remember that the mentioned test is a very ineffective tool when an older client is examined. The test will misinform the practitioner that tension in the costoveretbral joint(s) has built up, and the practitioner may believe he or she needs to reverse this state despite that is completely unnecessary.
The Erector Technique discussed in the article targets spinal erectors. The practitioner is supposed to use the elbow and forearm to apply vertical and caudal pressure when sliding along tensed erectors. This technique is helpful but only as an initial step, and the practitioner must apply pressure very carefully otherwise he or she will activate the client’s pain analyzing system and, as a reflex reaction, the same erectors will generate protective muscle tension and all efforts will go to waste. After careful application of Erector Technique, the practitioner should concentrate on the lateral displacement of the erectors instead of sliding up and down along the erectors.

Pes Anserine Group. Massage & Bodywork March/April, 47-48, 2012, by Christy Cael
It was great to see the term pes anserine, which in Latin means “goose foot,” in a massage publication. The only problem we have is the actual palpation part of the article. Unfortunately, only one-third of this article is correct. The picture in the article that is supposed to illustrate the correct way to palpate the so-called Pes Anserine Group shows only palpation of the gracilis muscle on the medial thigh. We are simply puzzled how the author was able to find and palpate sartorius muscle on the medial thigh while its belly is on the anterior thigh and how the semimebranosus muscle can be palpated on the medial thigh while its belly is on the posterior thigh. If members of the Editorial Board of Massage and Bodywork Magazine open any anatomy textbook, they will find that this article does not provide the correct information on this very simple subject.





The Arm Lines. Massage & Bodywork March/April, 98-105, 2012, by Thomas Myers
Great article! Highly recommended.





Brushing Up on Dental Worker Care. Massage & Bodywork March/April, 106-109, 2012, by Whitney Lowe
This is second article by the same author dedicated to occupational postural hazards associated with different professions. The previous article discussed the music profession and this current one is concerned with dental workers. The author deserves a lot of credit for bringing the issue of somatic pathologies associated with various professions to the front line of national publication.


Working With Hip Mobility. Massage & Bodywork March/April, 114-117, 2012, by Til Luchau
This is a very good and informative article on various techniques to restore and maintain hip mobility. We think that the author greatly diminishes the clinical value of the article by adding a section in which the same techniques are recommended for clients with total hip replacement. Despite that the article mentioned the danger and restrictions to the manual treatment, the overall impression left after reading the article is that it is routinely acceptable. We would like to emphasize here the danger of manual therapies mentioned in the article, and the necessity to work on these clients only after surgeon informed by practitioner in all details about treatment techniques and has granted permission (better written). It is a matter of grave importance especially to recognize that older clients, who have undergone total hip replacement and have weaker muscles, are sometimes unable to stabilize efficiently the endoprothesis.
Despite the article’s position on this matter, which we think is very unfortunate, we would like to warn practitioners about the potential dangers of using these techniques on clients with total-hip replacement. The unproven application of these techniques may easily hurt the client and consequently ruin a therapist’s practice. The author based his conclusion that it is acceptable to use these manual techniques on the reference to Yoga in which one-third of surveyed surgeons did not express any objections to Yoga practice after total-hip replacement. First of all, it is only one-third of the respondents and it is obvious that two-thirds did not share same views. And secondly, Yoga in which the client controls the movement is not the same as manual techniques in which the practitioner passively adjusts the hip joint. It is nonsense to compare Yoga with manual therapy.
Of course, our review can be seen by some readers as just our personal opinion. However, we encountered two similar cases in our clinic. Two of our new patients informed us that they had an unfortunate previous experience of the complete luxation of endoprothesis during passive stretching under different angles conducted during a regular massage session. In spite of our assurance that we do no such “therapies,” they were very anxious during their first treatment session until they felt that they were in the right place and not in any potential danger.
Here is what will happen if the practitioner incorrectly decides to use techniques discussed in this article. The hip will go out of the socket; the client will be in a lot of pain and completely unable to walk; an ambulance will be called to deliver the client in the nearest hospital; the patient will be immediately transferred into the operation room where, under general anesthesia, an orthopedic surgeon will place the hip bone part of endoprothesis back into the socket. For cases like this one, we suggest any practitioner has very good malpractice insurance before trying these techniques. However, it is up to the readers to follow or not to follow the recommendations in Luchau’s article.
Massage Therapy Journal




Massage & Autoimmune Disorders – What Can Research Tell Us? Massage Therapy Journal 51(1):87-89, 2012, by Martha Brown Menard, Ph.D., CMT
The article is a short review of available scientific data on massage and its effect on patients with autoimmune disorders specifically Lupus. Based on the lack of solid scientific data in this regard and usage of massage therapy on patients to maintain the quality of their lives, the author correctly emphasized several important points that we would like to reinforce:
1. Be careful when talking with the patient and promising actual improvement in their condition.
2. Do not use aggressive massage techniques. Never use deep tissue, compression or percussion on these clients
3. Do not work for an hour or one-and-a-half hours. Sometimes, especially at the beginning, even 30 minutes may trigger a flare up. The duration of the session can be slowly increased if there is positive clinical dynamic.
4. Design a symptom diary for your client, explain its importance and insist he or she keep this diary daily. The client should write down any new symptoms or changes in the old symptoms he or she experiences daily. Before each session, carefully read the diary and evaluate its contents. For example, after the last session, your client felt increased stiffness in the right shoulder joint. Be sure to spend less time on the right shoulder and use a combination of gentle repetitive effleurage in the direction of drainage and careful passive stretching during the client’s prolonged exhalation. The goal is to stimulate lymph drainage and unload packs of lymph nodes, which may be overwhelmed with waste products accumulated after the last session.




Body Mechanics. Facial Structure. Massage & Bodywork 51(1):73-77, 2012, by Dr. Joseph E. Muscolino
An excellent article on the anatomy and physiology of connective tissue. We highly recommend practitioners read it.


Massage Lupus. Massage & Bodywork 51(1):46-52, 2012, by Michelle Vallet
This is the second article on the effects of massage on clients with Lupus in the same issue of MTJ. It is written in a journalistic style with the absence of any scientific data or background, and based solely on the personal clinical experiences of a couple of massage practitioners who work with clients with Lupus. We do not think that the author was correct to use such personal experiences as a foundation for generalized clinical recommendations for therapists.
For example, it is completely wrong to use an hour-long session for the first treatment for clients with Lupus. Friction is a poor choice of technique especially at the beginning of the therapy. The lymph drainage system of any person suffering from Lupus is already overwhelmed with waste products formed because of autoimmune conflict. This is why the application of friction-that targets skin adhesions and additionally releases waste products, which are the remains of collagen, myoglobulin, glycoproteins, etc.-into the intracellular spaces where lymph forms is an unacceptable recommendation that may jeopardize the client’s health.
MTJ is the official publication of the American Massage Therapy Association, and is supposed to be a leader in the scientific exploration of massage therapy and, what is more important, in setting, at least, basic clinical guidelines for practitioners to follow. Instead, in the same issue we find two articles dedicated to the same topic of massage therapy used for the treatment of Lupus. Furthermore, each article offered different recommendations concerning the length of the session or intensity of the treatment. If the article by Martha Brown Menard, reviewed above, correctly recommends caution and careful approach to the treatment of clients with Lupus, then this article written by Michelle Vallet leaves the impression of a more aggressive approach to therapy.
Of course, the lack of solid scientific data means that both views may be expressed by MTJ but its experts should express the Journal’s own position on this issue. Instead, the Editorial Board chose to publish two articles with completely opposing views in the same issue without any Editorial comment. We are curious how the Editorial Board of MTJ sees the practical application of the information they publish when it gives conflicting recommendations and increases the confusion about an already confused topic.





Treating Without Diagnosing. Massage Magazine 51(1):26-29, 2012, by Dianne Polseno
This very important article is in response to a letter sent to MTJ with a question on how a therapist may stay within the scope of practice when making any diagnostic assessment of the client while, at the same time, being restricted by the nature of the massage therapy professional ethics.
We receive this same question frequently during seminars, in various blogs or in e-mails from practitioners. The author is completely correct when she says that legally the practitioner does not have rights or sufficient expertise to make a diagnosis and report it to the client. If the client comes to the office with an already established diagnosis, let us say Carpal Tunnel, the practitioner is in a very simple situation since all he or she needs to do is use the correct protocol to free the median nerve from the pressure.
A more complicated case, for example, may involve a client mentioning during questioning that he frequently feels a sensation of tingling and occasional numbness in the palm. What to do and how to explain it to the client?
The author provides ethically sound advice. Apply tests that confirm Carpal Tunnel Syndrome or, let us say, Anterior Scalene Muscle Syndrome, which may mimic clinical symptoms of the Carpal Tunnel. If you found that the tests you perform on the patient confirm your suspicion then your client is probably suffering from irritation of median nerve. Simply use the protocol you have already mastered without informing your client what exactly he has. Instead, you may say that: “The treatment I will use will help you eliminate your uncomfortable sensations.” If you always talk with your client about symptoms and how you are eliminating them using massage therapy you will be safe.
Massage Magazine




Best Face Forward. Massage Magazine 189, February: 22-26, 2012, by Bruno Chilky, M.D., D.O.
This is a very general review of Lymph Drainage Massage application on the face and neck to enhance the client’s physical appearance. In any scenario, if a practitioner would like to learn Lymph Drainage Massage, Dr. Bruno Chilky is the ultimate authority on this subject.




Massage Therapy Effect On Scars and Stretch Marks. Massage Magazine190: March: 26-28, 2012, by Pete Whitridge
A very good article that covers the nature of scars and stretch marks as well as basic information on massage’s treatment options. It seems that the author has much more valuable information to offer readers. Limited space or the journalistic style of articles published in Massage Magazine limit this important topic.
Category: Good Apples, Bad Apples
