In Part I of this article published in the previous issue of JMS (please go to Issue #2, 2012 of JMS), we discussed the pathophysiological aspects of most common types of headache. Parts II, III will cover the diagnostic evaluation of patients with migraine and tension-type headaches.
The tests discussed below are very simple, and extremely informative when done correctly. We use them on a daily basis on our patients and greatly appreciate their clinical value.
We would like to emphasize one important issue: The diagnoses the patients with chronic headaches labeled with are not written in stone. On a weekly basis, we see patients with migraine and headaches who had been diagnosed with anything from “Temporomandibular Joint Arthritis” to “Leakage of Cerebrospinal Fluid” and “Uncontrolled Chronic Migraine Unspecified Origin” that in reality have simpler explanations. Once correctly diagnosed, these patients were treated successfully with the MEDICAL MASSAGE PROTOCOL which we are going to discuss in Part IV of this article.
The reason for so many baseless diagnoses conducted in very respectful medical institutions was very simple: No one had applied the simple tests we discuss in this article and ruled out more obvious and frequently missed causes of headaches.
In this issue, we will concentrate on the examination of possible irritation and/or compression of the greater and minor occipital nerves. In the Part III of this article, which will be published in issue #4 2012 of JMS we will discuss the second part of diagnostic evaluation, which includes examination of the scalp and trigeminal nerve in cases of cluster headaches.
QUESTIONING
1. AURA
The first critical step in the evaluation of a patient with chronic headache and migraine is to find out if he or she had an aura that started before headache began. As we discussed in the Part I, an aura may have various forms from an unusual smell to visual changes. However, distortions of the visual analyzator are the most common form of aura. Usually, the patient who has had a true migraine with aura already knows about it. This is why the practitioner should ask first if the patient has an aura and specifically what type.
This information is important for two reasons: If the patient has an aura it means that he or she suffers from a true migraine. In this case, the best outcome of MEDICAL MASSAGE PROTOCOL is decreasing the intensity of migraine attacks, contrary to other forms of tension types of headaches, which can be completely eliminated by MEDICAL MASSAGE PROTOCOL.
Another issue is the kind of aura. The visual aura is more common and is frequently associated with more benign types of migraine while the auditory or olfactory auras are frequently associated with the most debilitating forms of migraine. In the latter case, the clinical outcomes of MEDICAL MASSAGE PROTOCOL are even more limited. The practitioner must discuss these issues with the patient before treatment starts. It is very important to present clearly the expected outcomes of the therapy with the patient so that he or she can make an informed decision about committing to the treatment course.
If patient does not know what the term “aura” means and has not discussed his or her headaches with a primary-care physician or neurologist, the massage practitioner must actively ask the patient during evaluation: Did you have changes in vision, unusual smells or noises before headache starts?
To summarize: The practitioner and client may expect complete control over the headache if an aura is not part of the clinical picture and irritation of greater and/or minor occipital nerve is real cause. If the patient has auditory or olfactory auras, it is less likely that the patient will obtain significant relief of symptoms.
2. HEADACHE LOCATION
This is an important part of the patient’s questioning. The practitioner must ask the patient about current (at the moment of interview) and any previouslocations of headaches. Let us discuss the most common locations of headaches, their clinical meaning and what to expect as a treatment outcome.
The patient indicates a headache located or originating on the back of the head in the occipital area especially in the area of the occipital ridge. This is an excellent prognostic sign for overall treatment success. The most common cause of this type of headache is tension in the posterior cervical muscles especially at their insertion along the occipital ridge. This tension can be with or without irritation or compression of the greater occipital nerve. If the occipital headache currently radiates or previously radiated to the head, and even to the eye, it is obvious that the greater occipital nerve is compromised. The practitioner should evaluate the degree of involvement of this nerve during manual examination of the patient, which we will discuss below.
The patient may have symptoms of the occipital headache as a result of increase or decrease of the blood pressure as well as drop in the glucose level. Recently, we witnessed an increase in the number of occipital headaches as a result of incorrectly designed weight-loss programs. Long Treadmill or Elliptical Machine exercises during which a person watches overhead placed TVs in the gym or reading a book require additional stabilization of the neck to concentrate the eyesight on one spot. Such overuse of posterior cervical muscles greatly contributed to their tension and the development of occipital headaches.
Frequently the same individual tries to watch his or her diet and, instead of diminishing the number of calories slowly, he or she does it very quickly. The sudden drop in the level of blood glucose becomes an additional factor that enhances the occipital headache. The patient must discuss correlations between headaches and fluctuations in the blood pressure or glucose level with primary-care physician.
A temporal headache can be triggered by the irritation or compression of the minor occipital nerve, Temporomandibular Joint Dysfunction or Temporal Arteritis. If the temporal headache originates or originated on the back of the head, irritation of the minor occipital nerve is more likely the cause. Evaluation of the patient with Temporomandibular Joint Dysfunction we discussed in the September-October 2010 issue of JMS.
The patient with temporal headache as a result of Temporal Arteritis has such severe pain that he or she will go to the emergency room first. However, if a diagnosis of Temporal Arteritis was established and the massage practitioner decides to work on the patient, the practitioner must completely avoid the temporal area. Pounding temporal headaches also can be triggered by fluctuations in the blood pressure.
When the patient complains about a widespread headache, which has a squeezing component, most likely the practitioner is dealing with a headache triggered by hormonal, metabolic changes or pathological changes in the balance of brain neurotransmitters. For these patients, MEDICAL MASSAGE PROTOCOL has very limited benefits.
Another possible cause is scarification and lost elasticity in cranial aponeurosis. This can be a side effect of the Greater Occipital Nerve Neuralgia. In this case, medical massage therapy, especially the scalpotherapy part of the protocol, can be a significant help for these patients.
Cluster headaches are identified by a one-sided pain around and behind the eye. The most common causes are Trigeminal Nerve Neuralgia or convergence phenomenon when compression of the greater occipital nerve by the posterior cervical muscle secondarily affects the supraorbital branch of the trigeminal nerve (see Part I of this article in Issue #2, 2012 of JMS).
The practitioner must clarify the existing connection by asking if the cluster headache was preceded by an occipital headache or if they occurred at the same time. The rest of the information the practitioner will obtain during palpatory evaluation.
The location of the pain in the area of the orbit is another important subject. If the pain is concentrated behind the eye, the practitioner may expect significant tension in the Tenon’s capsule, which like hammock supports the position of the eyeball in the socket. This diagnosis can be confirmed easily by a palpatory examination of the eye. In these cases, the practitioner must include eye treatment in the protocol. If the pain is more superficial and is located more around of orbit, the practitioner may skip the eye treatment and instead work around the orbit. Frontal or maxillary sinusitis may also trigger a cluster-type headache.
3. OTHER SYMPTOMS
The practitioner must learn what other symptoms the patient has in addition to headaches. Frequently, the intense headache overshadows other important symptoms that may give important diagnostic clues and affect the application of the MEDICAL MASSAGE PROTOCOL. The practitioner must ask if patient has or had sensations of tingling, numbness or burning pain over any areas of the scalp. This exact sequence of the symptoms reflects the intensity of irritation or compression greater or/and minor occipital nerve. From mild irritation (tingling sensation) to severe compression (burning pain) asking these questions allows the practitioner to obtain a general idea about nerve involvement prior of palpatory examination.
Another important question to ask is to describe the symptoms associated with cluster headache. Ask if the patient’s vision has changed recently (e.g., need for new prescription glasses, increase of astigmatism, etc.). The presence of these symptoms will indicate that the practitioner is dealing with a chronic, complicated case, and he or she needs the commitment for extra time from the patient. The practitioner should make this same conclusion in the case of the patient experiencing a nausea sensation at the peak of the headache.
4. PREVIOUS THERAPIES
What was used as a treatment option to control intensity of headaches is another important issue to clarify. Prescribed medications are not topic of this discussion. All patients with headaches and migraines use different medication from over-the-counter (e.g., Aleve or Tylenol) to opioid (e.g. Fentanyl or Percocet) and anti-seizure (Topiramate, Depakote) medications. The prescribed medication is an issue beyond the practitioner’s scoop of practice and, frankly, it is not as important especially at the beginning of the therapy since all medications patients used target pain itself.
The most common mistake the majority of health providers make, and that we observe on a daily basis, are attempts to “cure” the headache by blocking the pain-analyzing system instead of finding and addressing the origin of the headache. A headache is not a disease, it is a symptom or the outcome of something else, and finding and isolating the primary cause is the first critical step in the overall success of the therapy.
From this point of view, the following information can be helpful. If local injections of anesthetics along the occipital ridge, Botox injections in the same area or electric acupuncture have been used before and they gave the patient temporary relief, you can be assured that you may greatly help this patient using MEDICAL MASSAGE PROTOCOL. These modalities temporarily reduced the tension in affected cervical muscles, and they relax the peripheral nerve with a following decrease of intensity of the headache. The major disadvantage of these injections is the decrease in pain is temporary but the fact that they were temporarily effective is very good news for the patient.
PALPATORY EXAMINATION
For all four Compression Tests, the patient must lie on the stomach with his or her head slightly bent forward and placed on the forehead in a cradle.
1. EXAMINATION OF GREATER OCCIPITAL NEVRE
The greater occipital nerve is 3.8 +/- 1.6 mm in diameter and, as we discussed in the Part I of this article, it can be irritated or compressed in four areas starting from the superficial layer:
1. By the vertical portion of the upper part of the trapezius muscle at its insertion into the occipital ridge (see Fig. 1)
2. By the semispinalis capitis muscle below the occipital ridge (see Fig. 1)
3. By the oblique capitis superior muscle on the posterior-lateral aspect of the upper neck between the skull and transverse process of C1 (see Fig. 1)
4. By the oblique capitis inferior on the posterior-lateral aspect of the upper neck between the transverse processes of the C1 and C2 (see Fig. 1).
These areas are critical for the application of Compression Tests to determine where the greater occipital nerve is compromised.
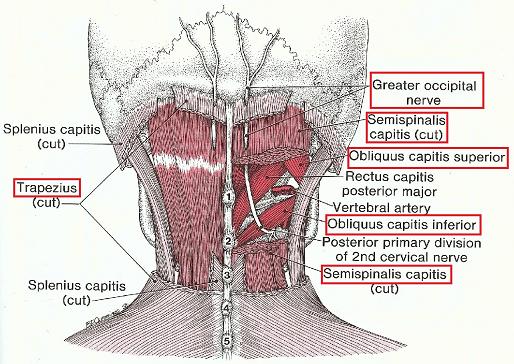
The Compression Test is applied just below the occipital ridge at the insertion of the trapezius muscle (see Fig. 1). First, locate the middle of the occipital ridge. It is easy to palpate due to its bony prominent part called external occipital protuberance (see Fig. 2). The Area of Compression Test application is located 1.5 cm laterally of the middle of the occipital ridge (Mosser et al., 2004).
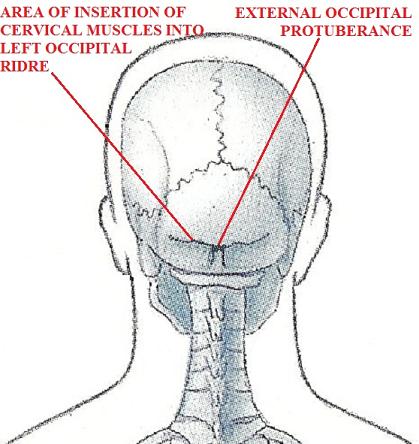
1 – area of application of the Compression Test at the insertion of trapezius and semispinalis captitis muscles into the occipital ridge
2 – external occipital protuberance
The next critical aspect for the correct execution of Compression Test is stabilization of the tendinous part of trapezius muscle before pressure is applied. The greater occipital nerve pierces the tendinous part of the trapezius muscle (see Fig. 1) and if, while applying the Compression Test, the tendinous part of the trapezius rolls medially or laterally under the thumb, the practitioner will miss the correct spot resulting in misleading test results.
The video below illustrates the location of the occipital ridge, middle eminence, the point where the trapezius muscle inserts into the occipital ridge and, finally, the correct and incorrect placement of the thumb to provide stabilization of the tendinous part of the trapezius muscle.
To stabilize the tendinous part of the trapezius muscle, first correctly identify its position. Place the thumb in parallel to the occipital ridge, slightly compress the tissue and roll the thumb back and forth with the skin just under the occipital ridge. You will feel the cord of the tendinous part of the trapezius muscle.
If the patient’s neck has an accumulation of subcutaneous fat, ask the patient to slightly lift the head up while resists it and tendinous part will immediately become prominent under the thumb. After determining that the thumb is on the tendinous part of the muscle, first apply vertical pressure to stabilize the tendinous part and prevent its rolling to the side.
The video below illustrates the stabilization of the tendon and the thumb slipping to the right or left when tendon rolls under it.
After you ensure that the thumb stays on the tendinous part of the trapezius, change the angle of pressure as shown in the last part of video above. Please pay attention to the position of the thumb and direction of applied pressure. Pressure must be moderate and increase slowly.
It is more informative if therapist slowly leans on the thumb with body weight instead of applying pressure from the thumb alone. In the latter case, part of palpatory sense is missed since the thumb is actively compressing the tissue while in the first case the pressure comes from the body to the stiffen thumb but the thumb itself does not work. It allows better evaluation of the tactile information from the thumb (e.g., if thumb stays on the tendinous part). The video below illustrate correct body mechanics.
The Compression Test is considered positive if application of moderate pressure causes severe pain (frequently described by patients as stabbing) under the thumb, and especially if pain radiates to the head or to the eye as in the cases of a cluster headache.
The most common mistake during execution of this Test is application of the direct vertical compression on the occipital ridge itself. In fact, this approach will elicit the exact same symptoms and the practitioner may see as a sign of greater occipital nerve compression by the trapezius muscle. However, in reality, the practitioner compresses the greater occipital nerve directly against occipital ridge after the nerve has already exited the trapezius muscle and is now positioned between the scalp and the skull. This area will be painful even in a healthy person because the nerve is compressed between the finger and the bone.
To prevent this misdiagnosis, the pressure needs to be applied just under the occipital ridge and directed to the occipital ridge at an angle of approximately 45 degrees. The video below illustrates this mistake.
To examine if the semispinalis capitis muscle (see Fig. 1) is irritating the greater occipital nerve move your thumb inferiorly along the same line, approximately 1cm lower than that point we discussed above (Ducic et al, 2009; Janis et al., 2004). There is no need to stabilize the tendinous part since your finger is on the flat muscle belly of the trapezius and semispinalis capitis muscle under it.
The video below illustrates the application of the Compression Test for the semispinalis capitis muscle. Pay attention to how the thumb goes under the occipital ridge with a combination of vertical compression and rolling while in the Compression Test for the trapezius muscle, discussed above, the thumb applies compression under the 45-degree angle without the rolling component. Be sure that thumb does not slide along the skin.
The test is considered positive if the patient feels pain under the thumb or pain radiates to the head and/or eye recreating the clinical picture of headache.
The most common mistake is application of direct vertical pressure, which does not reveal valued information about the condition of the nerve in the area where it pierces the semispinalis capitis muscle. The video below shows the incorrect application of this test.
The OCS is the short muscle that runs between the occipital ridge and transverse process of C1 (see Fig. 1). OCS rolls and tilts the head to the same side with unilateral contraction while during bi-lateral contraction it stabilizes the head, such as in cases when concentration of vision is required (e.g., working on the computer). This last action, which is pure isometric work, greatly contributes to tension in the OCS. As a result of spasms, the OCS misaligns the first cervical vertebra and pulls transverse process of C1 up secondarily affecting the greater occipital nerve and generating referred pain all way to the orbit on the same side (Fernandez de las Penas et al., 2005).
To apply the Compression Test for the OCS, position yourself laterally to the patient and place the tip of the thumb just below the skull from lateral direction. The video below illustrates application of Compression test for OCS.
In the video to the right of the thumb is the occipital ridge and in front and above is the edge of the cervical paravertebral muscles. Pay attention to the angle of pressure application. Increase the pressure slowly but the pressure must be significant to reach the OCS.
A frequent mistake is that the arm and hand applies too much vertical pressure. To correct this mistake and to get to right spot, lower the arm and hand to get to the correct angle. Please see video below.
OCI runs between transverse process of C1 and spinous process of C2. Its main action is head rotation to the same side with unilateral contraction and head stabilization during bi-lateral contraction.
First of all, the practitioner must find the spinous process of C1 that is the most prominent bone on the upper lateral neck. The oblique capitis inferior muscle is below the transverse process of C1. The greater occipital nerve, as seen at the Fig. 1, arches under the muscle, and its tension will irritate nerve and cause chronic headaches (Janis et al, 2010).
It is better to practice this test on a person with a longer neck and small layer of subcutaneous fat. The video below illustrates the application of Compression Test for OCI.
As you may see in the video, the tip of the transverse process of C1 can be located all way on the lateral neck while the patient is positioned on the stomach. After the tip of transverse process is identified, slide tip of the thumb inferiorly and slightly up and apply lateral pressure in the direction of vertebral column. Pressure must be mild since this area is sensitive in everyone. If mild pressure triggers pain and/or headache, the test is considered positive.
2. CLINICAL VALUE OF COMPRESSION TESTS
Compression Tests are very informative diagnostic tool. As it was shown by Zanchin, et al., (2001) even a self-administered application of CT has 86% accuracy and this percentage increases if tests are performed by a health practitioner.
Let us discuss how to interpret the information obtained during the application of Compression Tests. We have four potential areas where the greater occipital nerve can be compromised. The goal of palpatory evaluation is to detect the initial area of compression since this is where treatment needs to concentrate.
If, for example, the greater occipital nerve is irritated by the obliqus capitis inferior muscle, and since this area is the most deeply located, the compression tests will be positive in all three spots above it, because from the level of the oblique capitis inferior muscle the nerve is inflamed and ‘jumpy’ all way up to the insertion of the trapezius muscle into the occipital ridge.
During application of compression test between C1 and C2 on the oblique capitis inferior muscle, the application of pressure usually triggers the most uncomfortable pain and other sensations (e.g., tingling on the back of the scalp).
In another scenario, the Compression Test is positive just under the occipital ridge on the trapezius muscle, while the application of the Compression Tests to the semispinalis capitis and the oblique capitis inferior muscles are negative. In such case, the trapezius is responsible for the nerve compression and should be the primary target of the therapy. Thus, while examining these four areas, the practitioner has to find the area of compression that is located closest to the C1 spinal nerve from which the greater occipital nerve originates.
3. EXAMINATION OF THE MINOR OCCIPITAL NERVE
The minor occipital nerve is 1.2 +/- 1.6 mm in diameter and is smaller than the greater occipital nerve. Examination of the minor occipital nerve is simpler since this nerve can be found only in one area just below occipital ridge behind the mastoid process (see Fig. 3).
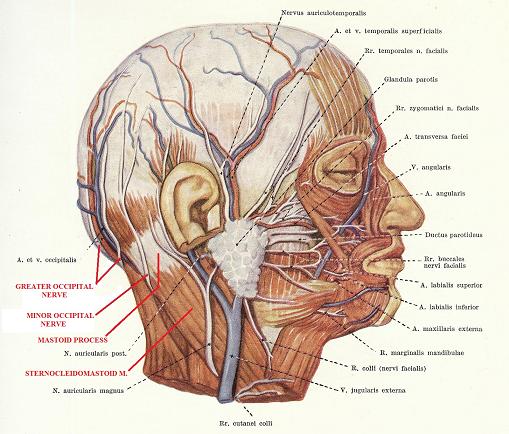
First, locate the mastoid process behind the ear. From the tip of the mastoid process its edge curves up and slightly posteriorly until it fuses with the lateral end of the occipital ridge. Exactly in the area of transition of the posterior edge of the mastoid process into the occipital ridge, the minor occipital nerve emerges behind the posterior edge of sternocleidomastoid muscle at its insertion into the mastoid process (Ducic et al, 2009). Here the minor occipital nerve lies on the occipital ridge just before continuing its pathway all the way to the temporal area. The video below illustrates the application of the Compression Test in the area of the minor occipital nerve.
Place your thumb as it is shown in the video and apply pressure just below occipital ridge with the slight lateral rotation of the thumb. The test is considered positive if patient feels sharp, stabbing pain under the finger or pain radiates all way to the temporal area.
Fernandez de las Penas C, Cuadrado ML, Gerwin RD, Pareja JA. “Referred pain from the trochlear region in tension-type headache: a myofascial trigger point from the superior oblique muscle.” Headache. 2000. 23:1830-1837
Janis J.E., Hatef D.A., Ducic I., Reece E.M., Hamawy A.H., Becker S., Guyuron B. “The anatomy of the greater occipital nerve: Part II. Compression point topography.” Plastic & Reconstructive Surgery. 2010 Nov; 126(5):1563-72
Mosser SW, Guyuron B, Janis JE, Rohrich RJ. “The anatomy of the greater occipital nerve: implications for the etiology of migraine headaches.” Plastic & Reconstructive Surgery. 2004 Feb; 113(2):693-7
Travel J.G., Simmons D.G. Myofascial Pain and Dysfunction. The trigger Point Manual. Williams&Wilkins, 1983
Zanchin G; Maggioni F; Granella F; Rossi P; Falco L; Manzoni GC. “Self-administered pain-relieving manoeuvres in primary headaches.” Cephalgia.21(7):718-26, 2001
Category: Medical Massage
