Massage therapy has a wide range of applications from stress management to sports massage and MEDICAL MASSAGE PROTOCOLs. It targets four types of soft tissue: skin, fascia, superficially and deeply located muscles, and the periosteum.
Depending on the final goal, different applications of massage therapy result in a variety of positive changes in the function of tissues and inner organs. However, as it was shown by Morelli et al., (1999), massage mostly contributes to the decrease of muscle spasm when the deeply located mechanoreceptors within the soft tissues are activated. These and other similar data clinically justify the application of deep tissue massage.
This article discusses four basic strategies for the application of deep-tissue massage (DTM). At the very beginning, I would like to state that from the massage science point of view, DTM is not a separate modality in how it is frequently practiced but rather a part of any clinical work whether it is stress management, medical or sports massage. Let us review four basic strategies for DTM: inhibitory regime of massage therapy, mobilization of the superficial soft tissue to expose deeper layers, shifting compression, and stretching of the superficial muscles while working on them.
1. INHIBITORY REGIME OF MASSAGE THERAPY
The inhibitory regime of massage therapy has two main clinical benefits: It inhibits the activity of sympathetic division (“fight and flight”) of the autonomic nervous system, activates the parasympathetic division (“rest and digest”) of the autonomic nervous system and suppresses the activity of the pain analyzing system if this system has been activated by somatic or visceral disorders.
In the healthy human, the sympathetic and parasympathetic divisions of the autonomic nervous system have very balanced relationships. For example, during exercise the sympathetic nervous system is activated. However, as soon as the exercise ceases, the parasympathetic nervous system becomes active and suppresses the activity of the sympathetic nervous system by gradually reducing the heart rate and respiratory rate.
In this way, the balance of the sympathetic and parasympathetic division of the autonomic nervous systems guarantees health. On the other hand, an imbalance of those systems is the initial trigger of chronic somatic and visceral disorders. Modern life is full of emotional and physical stresses, which trigger the increase of sympathetic tone every day. Thus, the inhibition of the sympathetic nervous system becomes a necessary step in restoring one’s health. A simple and effective way to do this is to use massage in the inhibitory regime using the proper pacing and rhythm of massage strokes.
Another equally important benefit of the inhibitory regime of massage therapy is its use as an initial step in the control of the pain analyzing system if it has been activated by a somatic or visceral abnormality.
Technically, the inhibitory regime of massage therapy means that the practitioner needs to apply massage strokes with the same speed, same moderate pressure, a consistent rhythm of 70-80 strokes per minute, in the direction of the venous and lymph drainage, and with the same combination of techniques (e.g., combine effleurage and kneading strokes). It is best to apply the massage over the targeted area for at least 2 minutes before the inhibitory regime will trigger the desired positive clinical outcomes.
Here is a scientifically based explanation of the clinical benefits of inhibitory regime of massage therapy. Every mechano- or proprioreceptor has its own level of adaptation assigned to the receptor by the central nervous system (CNS). The level of adaptation reflects the point at which the intensive stimulation of the peripheral receptors causes their failure to generate afferent (i.e., ascending) flow of impulses (i.e., action potentials) to the CNS.
With the prolonged application of massage in the inhibitory regime, the massive, continuous flow of harmless, ascending sensory stimuli from the massaged area reaches the CNS with following inhibition of the lower motor centers located in the spinal cord and upper motor centers located in the motor cortex. The inhibition of upper and lower motor centers triggers the inhibition of sympathetic nervous system.
Continuing massage in an inhibitory regime prompts the peripheral receptors to reach the level of adaptation. Adaptation is the inability of peripheral receptors to generate a new wave of sensory potentials destined for the CNS despite that stimuli in form of massage strokes continue to be applied to the massaged area. As a result of adaptation in the peripheral receptors, the spinal neurons in the posterior horns cease their stimulation of the motor centers in the anterior horns, and their inhibition triggers muscle relaxation and the decrease of the activity of the pain-analyzing system (Goldberg, et al., 1992; 1994).
While the events described above unfold and the inhibitory regime of massage therapy decreases the activity of the sympathetic division, the various clinical benefits are triggered that include local and general vasodilatation, lowering of blood pressure, decrease of stress-hormone production, etc.
The final benefit of working with the inhibitory regime is the relaxation of the soft tissues, which allows us to work into deeper layers of soft tissue. The layer-by-layer mobilization of the soft tissues allows the practitioner to reach deeper layers and allows us to stimulate a greater number of peripheral receptors. The more peripheral receptors we stimulate results in the client receiving the maximum therapeutic benefits of the massage.
2. MOBILIZATION OF THE SUPERFICIAL TISSUES TO EXPOSE DEEPER LAYERS
If tension has built up in the deep layer of the soft tissues, the practitioner should focus on that area, while trying to engage the upper layers of the soft tissue as least as possible. To do that, the practitioner should start with the inhibitory regime of massage therapy that we discussed above. For the next step the practitioner has two options: If it is anatomically possible, the superficial layers can be moved away to expose the underlying tissue. If it is impossible to move away superficial tissues, then the practitioner should work through them by mobilizing superficial tissues in the correct way using the shifting-compression approach.
Thus, our second strategy is to move superficially located soft tissue, especially the superficial skeletal muscles, to expose the deep fascia and muscles. To illustrate this concept, let us use as an example the massage of the rhomboideus major muscle without engaging the lower portion of the trapezius muscle, which covers the rhomboideus major by its free edge.
The rhomboideus major muscle originates from the spinous processes of T2-T5 thoracic vertebrae and the upper ribs, goes down and laterally and finally inserts into the lower part of the medial edge of the scapula. The fibers of the rhomboideus major muscle cross under the fibers of the lower portion of the trapezius muscle, and both muscles “hug” and stabilize the scapula along its medial edge.
Look at Picture #1 of the Fig. 1. The dotted line is the line of the spinous processes of thoracic vertebrae, the solid line is the medial edge of the right scapula and the dashed line is the free edge of the trapezius muscle that covers the rhomboideus major muscle.
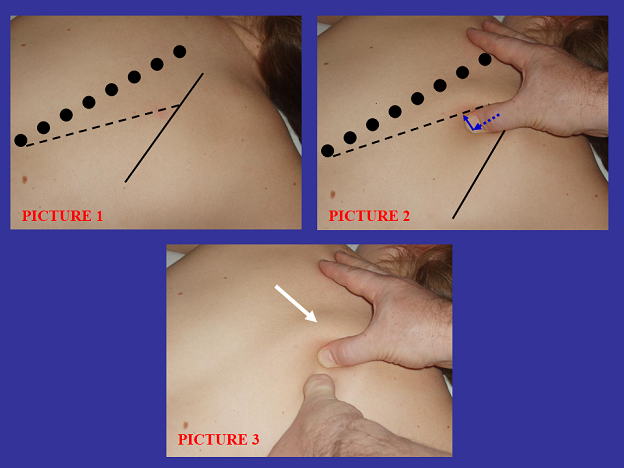
Fig. 1. Mobilization of the trapezius muscle to work of rhomboids major muscle
Picture #2 shows the therapist’s right thumb slightly pressed into the soft tissue in front of the free edge of the trapezius muscle (blue dashed arrow) and then pushed it medially in the direction to the vertebral column (solid blue arrow).
Picture #3 shows the trapezius muscle that is pushed medially and is seen on the picture as a bulge (white arrow) in front of the right thumb, while the left thumb works directly on the rhomboideus major muscle without engagement of the lower portion of the trapezius muscle, which is pushed medially.
In the same way, the upper portion of the trapezius muscle can be pushed aside in order for the practitioner to work on the levator scapulae and supraspinatus muscles directly, or the gastrocnemius is pushed away to work on the soleus muscle, or extensor digitorum muscle pushed away to expose supinator muscle, etc.
3. SHIFTING-COMPRESSION OF THE SUPERFICIAL TISSUE
The third strategy of deep-tissue work is used when it is anatomically impossible to move away the superficial layer of the soft tissue. In such cases, the practitioner must work on the deeper layer through the superficially located tissues.
The best example of this situation is with the piriformis muscle. The piriformis muscle originates on the anterior surface of the sacrum, exits the pelvis and inserts into the greater trochanter. The piriformis muscle is completely covered by the gluteus maximus muscle making it anatomically impossible to move its fibers away and work on the piriformis directly.
In order to address the piriformis muscle, we must first relax the gluteus maximus muscles using the inhibitory regime of massage therapy then apply enough pressure to compress the fibers of the gluteus maximus muscle and shift them up and forward holding them out of the way while apply massage techniques to as close proximity of the piriformis muscle as possible. Fig. 2 illustrates this approach. The practitioner works on the piriformis muscle thorough the fibers of the gluteus maximus using friction (Picture #1) and compression (Picture #2) while the majority of its fibers are shifted up (white arrows) exposing the piriformis muscle as much as possible.

Fig. 2. Shifting compression to the gluteus maximus muscle to address the piriformis muscle
4. STRETCHING OF THE MUSCLES WHILE APPLYING DEEP TISSUE MASSAGE
In some clinical cases the massage practitioner should stretch the tissue just before applying deep massage or while massaging the tissue. For example, when working on clients with tension in the masticatory muscles, which are responsible for TMJ dysfunction, the practitioner must apply deep-tissue massage. One of the techniques in these cases (see Fig. 3) is to passively open the client’s mouth (two blue arrows in the Picture #1 of Fig. 3) and hold it open to continuously stretch the masticatory muscle (one blue arrow in the Picture #2) while applying deep-tissue therapy.
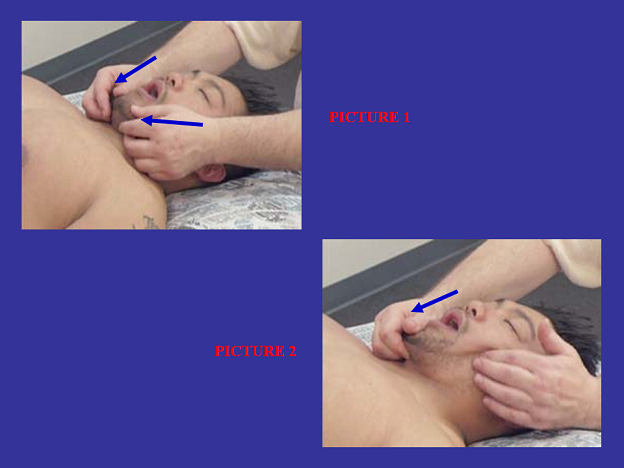
Fig. 3. Passive stretching of the masseter muscle while applying deep-tissue work
Another example of combining the passive stretching and deep-tissue therapy is work on the tissues affected by contracture. Usually contracture develops secondarily to the prolonged functional limitation of the normal range of motion. This is a very common side effect of long immobilization of a joint in a cast or various inflammatory pathologies (e.g. rheumatoid arthritis). Another cause of contracture is chronic spinal or peripheral nerve compression (e.g., Dupuytren’s contracture of the palmar aponeurosis due to the chronic compression of the median nerve in the Carpal Tunnel).
In cases of contracture, the combination of passive stretching of the tissue and deep-tissue friction and compression is the primary component of the Stretching Massage modality. The combination of these two important techniques in one treatment allows the restoration of the normal length and elasticity of the affected tissue and much deeper and successful mobilization.
CLINICAL BENEFITS
There are many clinical benefits to using deep-tissue therapy. It helps to eradicate local inflammation (e.g. Tendinitis), eliminates trigger point in the skeletal muscles (e.g., active trigger point in quadratus lumborum muscle) and periosteum (e.g., Tennis Elbow), increases the elasticity of scar tissue (e.g. after surgery), and restores ROM in cases of contracture (e.g., Frozen Shoulder).
However, there are additional, less known benefits of deep-tissue work associated with restoring normal bioelectricity in the soft tissue by generating piezoelectricity and streaming potentials (Turchaninov, 2000). While applying massage strokes in the correct way, the practitioner is able to activate the healing process by changing and restoring the normal bioelectricity in the soft tissue. To learn more about this fascinating mechanism of massage therapy please go to January/February and March/April issues of JMS or Therapeutic Massage. A Scientific Approach textbook.
These unique outcomes of deep-tissue work support long-lasting healing outcomes of therapy that remain with the client long after the therapy is finished.
HOW MUCH PRESSURE SHOULD BE APPLIED?
Frequently massage practitioners think that deep massage means applying greater pressure. This is an unfortunate misconception. There is no place for the “No Pain, No Gain” approach in scientifically sound massage therapy.
Of course, during deep-tissue massage, the practitioner uses more pressure than, let us say, during relaxing effleurage strokes. Nevertheless, applied pressure must follow four basic rules.
1. Pressure during deep-tissue work must be significant but always stays just below the client’s pain threshold. Given that pain is a very subjective sensation that varies from person to person or even from area to area in the same individual, we need to constantly correlate the amount of applied pressure to the client’s sensations.
2.To keep increasing pressure while applying deep-tissue work and staying below the client’s pain threshold, the practitioner should increase pressure in a “stop-and-go” approach. After each new addition of pressure in the treated area, the practitioner must give the client time to adjust to the new level of pressure before applying any additional pressure.
3.The practitioner should apply pressure to the level of the first pain sensations felt by the client. As soon as this point is reached the practitioner should slightly ease up applied pressure and work at this level until the client is ready for the next increase in pressure application.
4. Even if a client demands you continue to increase pressure after you have determined that his or her body has already generated protective muscular tension, you must reduce the pressure and restart the gradual increase of pressure application to avoid protective muscle tension.
Senseless application of strong pressure activates the pain analyzing system, generates protective muscle tension with following blockage of arterial blood flow and decreases venous and lymph drainage, which all will negate the clinical benefits of deep-tissue massage. If deep pressure is applied incorrectly and the practitioner continues to perform massage vigorously, he or she will additionally traumatize the muscles and fascia, causing their inflammation with the subsequent scarification and formation of myogelosises in areas where active trigger points are located.
With a gradual approach to the application of deep pressure in combination with continuous control of the pain analyzing system, practitioners are able to avoid injuries to the soft tissue while relaxing the superficial soft tissue and achieving access to the deepest levels of the soft tissue.
Goldberg, J ., Sullivan, S.J., Seabome, D.E. The Art of Stone Healing. Boca Raton, CRC, 2005.
Fleck D., Jochum L. The Effect of Two Intensities of Massage of H-Re?ex Amplitude. Phys. Ther., 1992, 72(6): 449-457
Goldberg, J ., Seaborne, D.E., Sullivan S.J., Leduc, B.E. The Effect of Therapeutic Massage on H-Re?ex Amplitude in Persons with a Spinal Cord Injury.Phys. Ther., 1994, 74(8): 728-737
Morelli M, Chapman CE, Sullivan SJ. Do cutaneous receptors contribute to the changes in the amplitude of the H-reflex during massage? Electromyogr Clin Neurophysiol. 1999 Oct-Dec;39(7):441-7
Turchaninov, R. Therapeutic Massage. A Scientific Approach. 2000, Aesculapius Books, Phoenix
Category: Stress Reduction Massage
