By Dr. Ross Turchaninov
We continue our series of articles under the general name, “How Massage Therapy Heals The Body” (please refer to issues of Jan/Feb, 2010; Mar/April, 2010; #3, 2011: #4 2011, JMS). In the previous issue of JMS (#3, 2014) we started a new topic: the modern science of pain from a massage therapy point of view. In Part I of this article we discussed the cornerstone of modern understanding of pain – The Gate Control Theory of Pain (GCT) developed by Professors R. Melzack and P. Wall in 1965.
In 1990 Professor Melzack made a new step in the science of pain by introducing the Neuromatrix Theory of Pain (NT). This theory was finalized in cooperation with another world renowned scientist, Professor J. Katz. The NT is the subject of this article and we would like to emphasize that this article must be read only after Part I, which was published in #3 issue of JMS.
Recently NT has created a wave of misunderstandings and misrepresentations in the community of somatic practitioners among chiropractors, physical therapists and massage practitioners. There is a significant chance that as some people read this article, they already have signed up or are waiting to take part in a seminar or webinar on the subject of pain and massage therapy. Our research shows that in many cases these continuing education classes are based on willing and unwilling misunderstanding and misrepresentation of NT. The situation had become so bad that we felt the need to get in contact with Prof. Melzack and Prof. Katz for clarifications of these important subjects for the community of somatic practitioners. We published their interview and our review of the current situation with GCT and NT in #4 issue of JMS.
Before addressing unscientific claims built around NT, we need to carefully go over the basic concept of NT. We will use the most frequently cited article on this subject as a source (Mezlack and Katz, 2013).
Despite that both theories are equally important components of our understanding of modern pain science, NT is more complex than GCT since it includes some philosophical concepts as well. We will try to explain simply, but it still requires the reader’s attention and ability to analyze scientific data. Please sit tight and follow the text and illustrations we provide. Here it goes:
THE ESSENCE OF NEUROMATRIX THEORY
After the formulation of GCT, Prof. Mezlack continued his scientific exploration of pain. Eventually he concluded that GCT doesn’t answer all questions clinical reality puts in front of scientists. The first step in building NT was the publication of the article by Professors Melzack and Loeser in 1978. In this paper the authors described cases of phantom pains developed in paraplegic patients after a trauma which caused complete section of the spinal cord.
Usually phantom pain as a clinical phenomenon is associated with pain in the limb after it was surgically removed due to severe trauma or cancer. In these situations the patient’s brain and spinal cord and peripheral receptors are still perfectly functioning together. Only what is lost is part of the limb. The patient feels phantom pain in this missing limb like it is still functioning.
However, in cases of paraplegic patients, the severe spinal trauma completely severed the spinal cord and the brain lost any chance of getting sensory input from the parts of the body below the spinal injury. Prof. Melzack and his co-author were puzzled by such a phenomenon. How can the patient’s brain form pain sensation in form of phantom pain below the level of injury when the brain had lost all communication with tissues there? The only explanation was that the brain on its own is able to generate pain without any sensory input from peripheral receptors. At that time it was truly a revolutionary idea!
Further studies and experiments conducted by Prof. Melzack and his associates allowed the formulation of a new step in our understanding of pain in the form of NT. Fig. 1 illustrates the concept and basic components of NT. This diagram has three parts: input to neuromatrix, neuromatrix with neurosignature and neuromatrix’s output to the different areas of the brain which produce various responses.
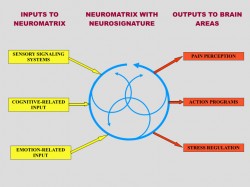
Fig. 1. Conceptual model of NT (Melzack, 2001)
1. INPUT TO NEUROMATRIX
As you can see in the left side of Fig. 1 (yellow squares) there are three major inputs into neuromatrix:
a. Cutaneous, visceral and musculoskeletal input (i.e., sensory signaling system).
This part of the input is the next step in the normal function of the Gate-Control System. As we discussed in Issue #3 of JMS, T-cells (or Transmissions Cells) in the posterior horns of the spinal cord transfer the sensory information they received from the peripheral receptors, including nociceptors located in the soft tissues, all way to the neuromatrix located in brain (see Fig. 2 in GCT article in Issue #3, JMS).
This is a very important segment of NT since some massage “educators” deny the peripheral origin of pain and insist on its solely central origin. We will address this issue later.
b. Memories of past experience, attention, anxiety (i.e., cognitive-related input).
This type of input is an absolutely revolutionary concept. Let’s say that the paraplegic patient during his years before spinal injury fractured his leg. Of course, during this traumatic event he experienced acute pain which eventually subsided during fracture healing. After he sustained the spinal cord injury and now the brain doesn’t have any sensory input from the extremity which once was broken, the patient suddenly starts to feel phantom pain in the leg in the area of fracture. In such case the memory of pain associated with the fracture was ‘imprinted’ into the neuromatrix and now the brain itself ‘recreates’ this pain in the form of phantom pain, despite that due to the spinal cord injury, there is not any communication between CNS and the once injured leg.
Similar explanations can be projected to situations well known to somatic practitioners. An excellent example is Fibromyalgia, which is a somatic abnormality with a very strong psychological or central component. In Fibromyalgia patients, long lasting chronic pain which initially originated in the soft tissues leaves its imprint in the neuromatrix. Now the brain starts to generate pain perception based on these previous pain experiences, in combination with anxiety and continuing pathological sensory stimulation from the affected soft tissues. Thus the chronic pain starts to feed on itself, devastating the patient’s life.
c. Stress which affects the limbic system (emotion-related input)
Acute or chronic stress has a devastating effect on the body. According to a revolutionary concept by Prof. H. Selye’s called General Adaptation Syndrome (1955), modern medicine sees chronic mental, emotional and physical stress as major factors in the development of various somatic and visceral disorders in our body.
The first negative outcome of stress is excessive activation of the sympathetic nervous system and release of cortisol into the blood stream. It is a normal body’s protective response to any type of stress. However, the constant increase of cortisol level associated with chronic stress has a devastating effect on the body. Cortisol elevates blood sugar, breaks proteins in the skeletal muscles and suppresses the immune system.
“Sustained cortisol release, therefore, can produce myopathy, weakness, fatigue, and decalcification of bone… it suppresses the immune system”.
(Melzack and Katz, 2013)
These effects contribute to the chronic pain and are especially important since part of the brain’s limbic system called the hippocampus is responsible for breaking active cortisol. Changes in the limbic system due to negative emotions associated with pain and stress exhaust the limbic system and decrease its ability to break cortisol and maintain its normal level in the blood stream.
Conclusion: these three inputs to the neuromatrix equally contribute to the final formation of pain perception by the brain. In all cases of chronic pain, these inputs act at the same time by contributing to the formation of overall pain perception.
2. NEUROMATRIX AND NEUROSIGNATURE
The middle part of the Fig. 1 (blue circles) illustrates the position and role of the neuromatix in brain function, formation of pain and other ouputs. First let’s define what the neuromatrix is. According to Prof. Melzack and Prof. Katz (2013) the neuromatrix is a “widespread network of neurons that consists of loops between the thalamus and cortex as well as between the cortex and limbic system”
Thus the neuromatrix is located in the upper echelons of the CNS. Its neurons unite three critical parts of the brain: the thalamus, which is a major relay station to determine what part of the cortex must be activated and by what stimuli; the limbic system, which controls our emotions; and the cortex as a mainframe computer which creates motor output to control body functions. These neural loops are shown as the circular arrows in the middle part of Fig.1.
So how does the neuromatrix work? As a result of various events we discussed above in the left side of Fig. 1, the neuronal loops of the neuromatrix are activated and they start parallel production of cycling nervous impulses. This cycling synthesis and processing of information allows the neuromatrix to produce in parallel several possible pattern of action as a response to the stimuli. The unsuitable ones are eliminated one by one until the most appropriate for these particular circumstances emerges.
In a sense, the neuromatrix is a system which helps the brain to quickly eliminate wrong choices and find the best answer to the multi-choice question which it encounters every second of our lifetimes. All our experiences like chronic pain, jealousy, envy etc., have their imprint in the neuromatrix and these existing imprints can be easily activated by new sensory triggers or past memories or emotions.
Prof. Melzack and Prof. Katz called these areas of the neuromatrix associated with chronic pain, various emotions, past memories or analyzed sensory inputs – neuromodules. These neuromodules compose the combined output of the neuromatrix which is synthesized there and it is called a neurosignature.
Another critical role of the neuromatrix is the formation of our body self-awareness. Millions of various factors from basic sensory stimulation of the skin to previous pain memories or long ago negative emotions and stress leave their imprint in the neuromatrix and it produces various sensations from sensing temperature change to chronic pain.
For example the person who feels chronic pain as a result of injury also feels fluctuation in surrounding temperature, body position at this moment, the pressure of a chair, the smell of the food, the ring of a cell phone, etc. Let’s say that the same individual who suffers from chronic pain while sitting at a table suddenly sees images of a car crash on TV. It reminds him of his own car accident and trauma and at this moment he feels that his pain is getting worse.
Prof Melzack and Prof. Katz made the following analogy for the neuromatrix’s role in forming our body self-awareness.
“Like violins and brasses of a symphony orchestra where each comprise a part of the whole; each makes its unique sound contribution yet is an integral part of a single symphony which varies continually from beginning to the end.”
Conclusion: Thus, all our experiences from hot/cold sensation to pain are synthesized by our brain in the form of a neurosignature, according to the initial triggers which are presented in the left part of Fig. 1. This neurosignature is continually projected to the corresponding parts of the brain creating body self-awareness which allows us analyze and fully interact with the very complex reality surrounding us.
3. OUTPUTS TO THE BRAIN
The right side of the Fig. 1 (red squares) illustrates various outputs of the neurosignature to the brain.
a. Pain perception
According to Prof. Melzack and Prof. Katz, pain perception synthesized by the brain includes sensory, affective and cognitive dimensions and thus is a very complex output.
b. Action programs
Action programs include voluntary actions like our movements and involuntary like gastric juice secretion when we are hungry.
c. Stress-regulation programs
Body response to acute or chronic stress is very important output. It includes regulation of cortisol, noradrenalin, dopamine, endorphin production and the immune system’s activity.
Conclusion: The final output to the brain is the result of complex interactions of initial triggers delivered to the neuromatrix by the Gate Control System or originated in the neuromatrix itself.
This very short review of the Neuromatrix Theory is based on publications by Prof. Melzack and Prof. Katz (2013). One more time we would like to emphasize that according to the authors of NT, it describes events in the brain itself after the Gate-Control mechanism has already been activated and finished its role in the formation of the pain perception.
PROFESSOR G.L. MOSELEY’S WORK
The Neuromatrix Theory of Pain in the beginning of 21st Century greatly impacted modern medicine the same way the Gate Control Theory of Pain did in the middle of 20th Century. NT gave birth to many great clinical ideas which improved our ability to understand and control the patient’s pain-analyzing system. One example is the work of Australian neurologist Professor G.L. Moseley, who deserves a lot of credit for his contribution to the science of pain.
Unfortunately, his work was incorrectly generalized by many somatic practitioners, including chiropractors, physical therapists and massage practitioners, and as a result many unscientific ideas started to widely bloom especially within the massage therapy community. These ideas were immediately picked up by ‘educators’ who started to spread them via seminars and webinars confusing practitioners and diminishing the clinical value of massage therapy. Before we discuss this subject we need to discuss Prof. Moseley’s work and his contributions to pain science.
Prof. Moseley’s work is mostly based on NT developed by Prof. Melzack. Prof. Moseley concentrated on the critical role the brain itself plays in the formation of pain perception. His studies confirmed that to successfully control the pain analyzing system practitioners must take into account various neurological events within brain.
He and his co-authors are completely correct since any chronic pain carries a significant so-called central component. In some category of patients, e.g., phantom pains, Complex Regional Pain Syndrome, Fibromyalgia, etc., the central component of pain eventually starts to play the leading role in pain that patients suffer from.
Besides studying and examining the role of the brain in pain perception, Prof. Moseley also developed clinical tools to help medical professionals address the chronic pain. He developed the Graded Motor Imagery (GMI) treatment which includes three major psychological techniques:
1. Left/right discrimination training – helps patients in chronic pain restore normal recognition of left and right sides associated with the areas of their chronic pain
2. Motor imagery exercises – a brain exercise when the patient in chronic pain repeats imaginary movements of the affected parts without actual movements
3. Mirror therapy – is a very interesting technique which was originally developed by Dr. V.S. Ramachandran for patients with phantom pains (see Fig. 2).

Fig. 2. Original concept of Mirror Therapy developed by Dr. V.S. Ramachandran
The patient puts the stump (amputated left forearm in the Fig. 2) behind the mirror and places a good limb in front of the same mirror. The patient looks into the mirror and now sees both the good limb and its reflection which seems that the patient has now both limbs intact. While moving the good limb, he now also sees movements of the lost limb. At this moment the combined activation of the visual cortex and proprioceptors allows temporary elimination of the phantom pains in the amputated limb and with repetitive application it helps patients to deal with this debilitating condition.
Prof. Moseley also dedicated his research time to examine a variant of Mirror Therapy called Rubber Hand Illusion (RHI). RHI is also a fascinating technique and let’s go over it with the help of Fig. 3.

Fig. 3. Rubber Hand Illusion
The healthy individual sits with left hand hidden from view behind the solid screen and a rubber hand is placed on the table instead of the real left one. The other real hand is on the table but it is separated by the screen from the fake one. If the practitioner simultaneously strokes the fake hand and the real one, the subject will feel similar sensory stimulation in both hands – real one and rubber one – despite that the real hand wasn’t stimulated and it is hidden from view.
This simple experiment opens great clinical possibilities. If RHI has such impact on the brain it may be possible that let’s say the patient with chronic hand pain may get relief from RHI. As it was shown by Prof. Moseley (2005), this is exactly the case. The patients with Complex Regional Pain Syndrome indeed obtained pain relief with Prof. Moseley’s psychological interventions.
Thus, Prof. Moseley deserves a lot of credit for his contribution to pain science. However, he works with a special group of patients who have a great central component of pain, like phantom pains or Complex Regional Pain Syndrome. There is no doubt that these techniques are extremely beneficial to those patients. However, this isn’t the case when the patient has chronic pain as a result of various somatic or visceral abnormalities.
Unfortunately for somatic rehabilitation, several ‘educators’ took Prof. Moseley’s work literally and generalized it in all cases of chronic pain, considering that it has only a central component. It completely undermines the basic concept of Gate Control Theory and Neuromatrix Theory which emphasize the critical role the peripheral component plays in the formation of pain perception. First of all let us quote Prof. Moseley since his work is actively cited and misused by the proponents of these ridiculously unscientific ideas and any counter-argument is labeled as “outdated science.” These are quotes from articles Prof. Moseley co-authored:
“…there is limited systematic evidence, and the paradigm (mirror therapy by JMS) appears to be counterproductive during early rehabilitation.” (Giummarra, M., Moseley, L., 2011).
“In two experiments, undertaken by independent research teams and both powered to detect a clinically relevant effect, we failed to detect any modulation of pain thresholds, nor of pain evoked by individually calibrated high and low painful stimuli, in association with the rubber hand illusion.”
and
“This finding suggests against the utility of the rubber hand illusion as a therapeutic tool for pain relief in a clinical setting…” (Mohan R, Jensen KB, Petkova VI, Dey A, Barnsley N, Ingvar M, McAuley JH, Moseley GL, Ehrsson HH., 2012).
Also, several studies analyzed scientific data regarding clinical application of these techniques and concluded that they do not produce stable clinical results when they are used in clinical practice as the only treatment tool.
“There is a moderate quality of evidence that Mirror Therapy as an additional intervention improves recovery of arm function, and a low quality of evidence regarding lower limb function and pain after stroke. The quality of evidence in patients with complex regional pain syndrome and phantom limb pain is also low. Firm conclusions could not be drawn.” (Rothgangel et al., 2011).
“There is presently little evidence describing the value of the rubber hand illusion and virtual hand illusion as indices in the diagnosis or treatment of different pathologies…” (Christ and Reiner, 2014)
So when should the psychological techniques examined and developed by Prof. Moseley be used? The possibilities are countless: negative body image and loss of body ownership (Lenggenhager et al., 2014), body dysmorphic disorders (Kaplan et al., 2014), robotic hand ownership (Caspar, 2014), etc. It is obvious that all of these fields of application are beyond massage therapy’s scope of practice.
Despite that modern science proved that treatment based on central only component of chronic pain is misleading concept, several ‘new” massage methods which are based on the same notion were proposed. For example, Dermoneuromodulation, which is a combination of well-known medical massage techniques of nerve stretching and skin mobilization scarcely put together and simply re-named as a new modality.
Could techniques advocated by Prof. Moseley be used by somatic practitioners? Absolutely! However, they should be used in combination with correctly designed MEDICAL MASSAGE PROTOCOLs in an integrative concept rather than used alone or as a silver bullet for all cases of chronic pain we as humans experience. We will discuss these topics in last part of this article in the next issue of JMS.
REFERENCES
Butler, D. S., & Moseley, L. S. (2003). Explain pain. Adelaide: NOI Publications. Dudai, Y. (1989). The neurobiology of memory. Concepts, findings, trends. Oxford: Oxford University Press.
Caspar EA, De Beir A, Magalhaes De Saldanha Da Gama PA, Yernaux F, Cleeremans A, Vanderborght B. (2014) New frontiers in the rubber hand experiment: when a robotic handbecome one’s own. Behav Res Methods.
Christ O, Reiner M. (2014) Perspectives and possible applications of the rubber hand and virtual hand illusion in non-invasive rehabilitation: technological improvements and their consequences. Neurosci Biobehav Rev. Jul, 44:33-44.
Giummarra, M., Moseley, L. (2011), Phantom Limb Pain and Bodily Awareness: current concept and Future Directions., Current Opinion in Anesthesiology 24: 524–531.
Kaplan RA, Enticott PG, Hohwy J, Castle DJ, Rossell SL. (2104) Is body dysmorphic disorder associated with abnormal bodily self-awareness? A study using the rubber hand illusion. PLoS One. Jun 12;9 (6):e99981.
Lenggenhager B, Hilti L, Brugger P. (2014) Disturbed Body Integrity and the “Rubber Foot Illusion”. Neuropsychology. Sep 29.
Melzack R. (1990) Phantom Limbs and The Concept of Neuromatrix. Trend Neurosci.. 13:88-92.
Melzack, R., Katz J. (2013) Pain. Wiley Interdisciplinary Reviews: Cognitive Science, 4(1):1-15, Jan/Feb., 2013
Melzack, R. (2001) Pain and the Neuromatrix in the Brain. J. Dental Ed., 65:1378-1382.
Melzack, R, Loeser J.D. (1978) Phantom Body Pain in Paraplegics: Evidence for Central ‘Pattern Gathering” Mechanism” for Pain. Pain, 4:195-210
Moseley G.L. (2005) Is successful rehabilitation of complex regional pain syndrome due to sustained attention to the affected limb? A randomized clinical trial. Pain. Mar;114(1-2):54-61.
Mohan R, Jensen KB, Petkova VI, Dey A, Barnsley N, Ingvar M, McAuley JH, Moseley GL, Ehrsson HH. (2012) No Pain Relief with the Rubber Hand Illusion. PLoS One. 7(12):e52400.
Rothgangel, A.S.; Braun, S.M.; Beurskens, A.J.; Seitz, R.J.; Wade, D.T. (2011). The clinical aspects of mirror therapy in rehabilitation: a systematic review of the literature. International Journal of Rehabilitation Research 34 (March): 1–13.
Selye, H. (1955). Stress and Disease. Science 122: 625–631.
Category: Medical Massage
