During the Medical Massage seminars conducted by SOMI, our students ask about the value of dissection courses. We think this is a critically important component of the profession that unfortunately is missed in most therapists’ education. Thus every dissection course is an excellent way to improve your clinical skills. Pictures or plastic models are not a substitute for the valuable information therapists get during dissection courses. Therapists in Ireland and Great Britain are even luckier since they can learn from anatomist John Sharkey. In this issue we start the publication of his articles on BioTensegrity.
Dr. Ross Turchaninov, Editor in Chief
CONCEPT OF BIOTENSEGRITY
PART 1. THE FALLACY OF BIOMECHANICS
By John Sharkey, Clinical Anatomist. MSc.
Department of Clinical Sciences,
University of Chester/NTC, Dublin , Ireland
Introduction
The BioTensegrity concept is emerging as one of the most significant developments in human anatomy in recent years. It has important ramifications for a wide range of medical practitioners including surgeons, bio-engineers, medical massage practitioners and human movement specialists. Bespoke dissection techniques are providing a new vision and understanding of the continuity of the human form. A fresh look at the human fasciae highlights its role in providing continuous tension throughout the entire human body.
The term “Tensegrity” was coined by B. Fuller, combining the words “tension” and “integrity.” Further work continued by Fuller’s student, K. Snelson. Dr. S. Levin, an orthopedic surgeon, was the protagonist for “BioTensegrity” as early as the 1970s.
As a Clinical Anatomist, I have studied this model and the role of fascia in my fresh-from-frozen cadaver dissections to better understand the mechanisms of human movement and chronic pain while providing new anatomical knowledge and awareness leading to less invasive surgical and non-surgical therapeutic interventions. This new anatomical awareness is essential for medical massage practitioners to be clinically effective while treating various somatic pathologies.
Understanding BioTensegrity
In the BioTensegrity model the limbs are not a simple collection of rigid body segments held together by soft tissues. In anatomical reality the upper and lower limbs consist of semi-rigid, non-linear, viscoelastic segments. Viscoelasticity is the ability of the tissue to exhibit both viscous and elastic characteristics under applied pressure. These segments are interconnected by non-linear connectors like cartilage, joint capsules and ligaments, which in turn are integrated with the active motor system which includes the muscles and tendons.
The BioTensegrity model counters the widely accepted notion that the skeleton is a frame for the soft tissues to hang upon. This outdated concept can be easily illustrated by the following analogy between biomechanical forces which affect the human body and freely standing columns.
Imagine the column whose center of gravity is constantly changing while its base is rapidly shifting horizontally. Such a column would require great forces for its stabilization. These forces become incalculable if the column we imagine is composed of several rigid segments (bones), hinged together by flexible connectors (joints).
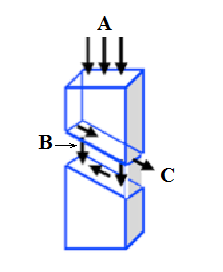
Fig. 1. When vertical loads are applied, the compression and shear stress forces oriented obliquely developed within connectors (Levin 1995. With permission).
A – vertical loads
B – compression forces
C – shear forces
An additional compromising factor for such a column would be its own weight, which creates internal shear forces in the flexible connectors (Fig. 1) contributing to further destabilization. If we look at our body from such an outdated view, our body will act like this column while we are in a vertical position. Thus it is obvious that if the concept of the skeleton frame were correct, our body would require a great amount of energy just to stabilize itself at rest in the vertical position.
In contrast, the concept of BioTensegrity sees the body as a self-tensioned, continuous myofascial network with floating skeleton structures contained within. Like all biological organisms, the human body is a multi-directional structure. For the system to always function efficiently, regardless of the direction of applied force, the tension elements (soft tissues) must constantly maintain necessary tension, while the function of compression elements (bones) is to “float” in a tension network developed and maintained by the soft tissues (Levin 1995).
No Bones About It
Brittleness, stiffness and strength of bones is roughly the same in all animals. However, if we look at the skeleton simply as a frame, horses while running or jumping on their slim limbs would break and fracture bones. For years we made the same mistakes. We applied the linear laws of mechanical physics which governs the behavior of non-biological materials under stress to living organisms! If we continue to do that, we need to find a reasonable explanation why animals as big as a rhinoceros are not collapsing under their own weight since animal mass must cube as its surface area is squared.
Thus the live tissues are able to work elastically at strains about a thousand times higher than strains ordinary technological solids can withstand. It proves that biological tissues behave differently than non-biologic materials.
If we use simple mechanical laws trying to explain complex relations which the force of gravity and tension elicit on our bodies, than the skull should eventually explode with heart beats due to the blood vessels expanding and crowding out the brain; as the urinary bladder filling up its thin walls should eventually burst; the pregnant uterus should rupture with the contractions of delivery (Levin, 1982).
Since biologic tissues, including muscles and fascia, have nonlinear stress/strain arrangements, we can’t use laws of hard matter linear physics while trying to explain and describe complex physiological events constantly happening in living organisms. However, this is exactly what modern biomechanics and kinesiology do and this flawed approach continues to be distributed to students of various health schools. Seeing ligaments, cartilage and bones as a simple system of ropes and sticks acting as different leverages is an absolutely incorrect approach since they would do little to support our upright functions if not for the collective activity of an integrated myofascial system.
The Cellular Level
To fully understand and appreciate fascia and its functions we need to start at the cellular level. There are exciting new discoveries in this field. For example, we now know that fascia contains a special water-filled vacuolar system that is capable of sliding independently to the rate of the muscle contractions. Vacuoles are enclosed compartments filled with water containing various inorganic and organic components. This system is also capable of facilitating and supporting capillaries throughout the fascia (Guimberteau, et al., 2010).
The fresh frozen cadaver image (see Fig. 2) of the deep fascia illustrates a macroview of this vacuolar structure with a supportive system of a fascial network. In the picture you see fresh frozen cadeveric specimen with looks like a chaotic arrangement of deep fascia fibers in the anterior forearm. Such an arrangement contributes to the stretching capability of the tissues. The vacuolar system is located within this network.
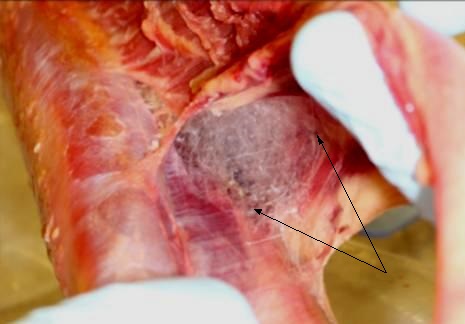
Fig. 2. Fresh frozen cadaver specimen of anterior forearm (Sharkey, 2010)
Arrows – vacuolar structure embedded into the supportive fascial network
This vacuolar structure has very interesting capabilities. It is able to change the shape while compressive tension is applied and return to its original state, while continuing to maintain same volume. The presence of a vacuolar system in the fascia provides a stable, yet flexible environment necessary for fascia to act as a force and tension transmitter (Huijing, 2009).
The new biomechanical model which is based on the concept of BioTensegrity, identifies fascia as the tensional, continuous member of the body. In a sense, the continuous tensile forces originated within the myofascia tissue form an “ocean” within which the bones float.
In the BioTensegrity model the bone structures do not transmit pressure force directly onto each other, since they are not continuous. Instead, the pressure between bones is transmitted via myofascial components. Since in contrast with bone structures, myofascial tissues are continuous. They equally distribute tension load directly to all other tensional members, bones, cartilages (Fuller, 1961). Eventually the fascial ocean of our bodies becomes seas, lakes, rivers and streams, while the tensility forces spread throughout it (Sharkey, 2008).
Thus, the Newtonian model of linear mechanical forces is the basis for the description of all things of non-biological nature (Levin 1995) while the same model isn’t acceptable for studying and describing the tensile and tension transmitted properties of living tissues.
The BioTensegrity model sees connective tissues differently since it recognizes fascia as a source of a wide network of communication (Schleip and Muller, 2013) linking left side to right, front to back, top to bottom, embracing and permeating the entire body. The strong visual record of the continuity of the superficial fascia throughout entire human body is shown in Fig. 3 (Sharkey, 2012).
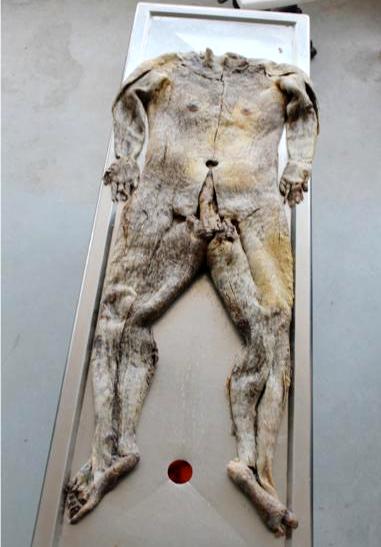
Fig. 3. A view of the superficial fascia removed as one autonomous structure (Sharkey, 2013)
The BioTensegrity model sees any tension change anywhere within the myofascial system as a whole body event. For example, middle back tension is instantly signaled to everywhere else in the body and a total body response is triggered via change in mechanical transduction which spreads throughout entire myofascial system. Thus the fascia translates tension signals into a whole body communication system. Such connective tissue signaling would be affected by changes in posture and movements as well as by various pathological conditions or when one experiences pain (Langevin, 2005, Purslow and Delage, 2012).
Since connective tissue structures create the framework of the visceral organs and they are also supported by connective tissue structures, the visceral organs become structurally and physiologically integrated into the myofascial system as well. Due to such an intimate intrinsic relationship that connective tissue has with the lungs, intestines, heart, spinal cord and brain, connective tissue signaling may have a reciprocal influence on the functions of different organ systems.
Fig. 4 illustrates the septa originated from the deep fascia and attached all way to the skin. This is one example of how connective tissue signals spread the tension between tissues and parts of the body.
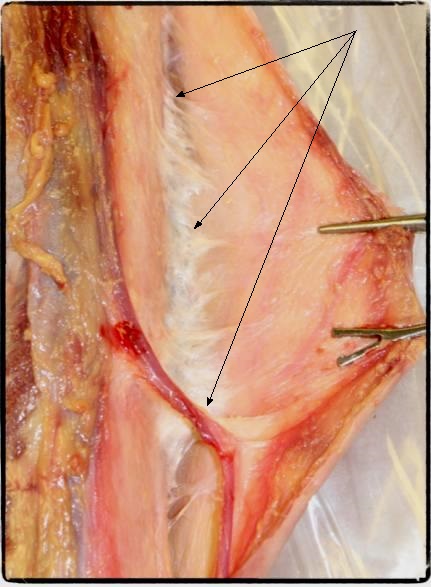
Fig. 4. Strong septa from the deep fascia are exposed as the skin and subcutaneous tissue are
distracted (Sharkey, J. 2013)
Arrows – fibers of the deep fascia
Fascia plays an important role in supporting muscle contraction since it links muscles and non-muscular structures by means of myofascial pathways (see Fig. 5) and by direct attachment of muscles into the connective tissue structures around the joint.
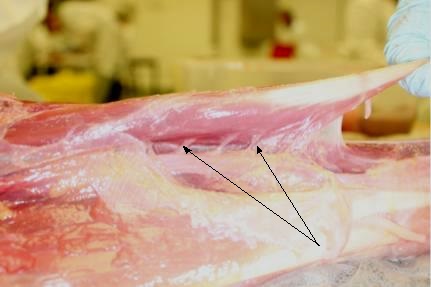
Fig. 5. Fascial collagenous links between Palmaris Longus and associated neighboring muscles.
(Photo Sharkey, J., 2012)
Arrows – fascial links
None of the muscle fibers insert directly into the bone but they use the connective tissue apparatus which provides stabilization at the insertion of the tendinous part of the muscle into the periosteum (Van der Wal, 2009). Additionally, these areas where the stress is the highest are very rich with various nerve endings and this additionally complicates situations when tension is spread unequally.
Fascia – A Question of Proprioception
Proprioception is our knowledge of where the different parts of body are and how much force is needed to execute movements. Until recently the function of proprioception was solely attributed to muscles, ligaments and tendons. However, several studies have confirmed the presence of a wide variety of sensory receptors and neural pathways within the fascia.
Van der Wal (2009) concluded that fascia has almost 1000% more sensory nerves when compared to muscle. Thus many authors started to see fascial structures such as membranes, septa, deep and superficial fascia as a major players in the formation of our proprioception and pain perception in the brain (Schleip, 2003, Stecco et. al., 2007, Standring 2008).
It was argued that tensional forces while spreading in several directions throughout a continuing “ocean” of connective tissue activate proprioceptors which provide the necessary feedback for the execution of the most efficient and economical movements, even in distant parts of the body (Stecco et. al., 2008).
Thanks to the BioTensegrity model, a different vision of anatomy and biomechanics is emerging. Understanding the dynamic and continuous relationships between the connective tissue structures and muscles, tendons, blood and lymphatic vessels, nerves and inner organs opens new exciting professional opportunities for somatic therapists. This vision encourages therapists to see their work as a whole body intervention instead of local treatment of a individually tensed muscle or inflamed tendon.
In part 2 of this series:
John Sharkey will discuss BioTensegrity, Four Bar Linkage and Guided Stress Transfer (GSF) with Clinical Implications for Medical Massage and movement therapies.
REFERENCES
Fuller R. B. Tensegrity. Portfolio and Art News Annual, No.4, 1961
Guimberteau J, Delage J, McGrouther D, Wong J., 2010. The microvacuolar system: how connective tissue sliding works. J Hand Surg Eur., 35(8):614–622.
Huijing, P. A., 2009. Epimuscular force transmission: a historical review and implications for new research. International Society of Biomechanics Muybridge Award Lecture, Taipe, 2007. Journal of Biomechanics. 42(1), 9-21.
Langevin, H. M., 2008. Potential role of fascia in chronic musculoskeletal pain. In J. Audette, and A. Bailey (Eds). Integrative pain management: The science and practice of complementary and alternative medicine in pain management. (pp. 123-132). New Jersey, USA. Humana Press.
Levin, S. M., 1982. Continuous tension, discontinuous compression, a model for biomechanical support of the body. Bulletin of Structural Integration, Rolf Institute, Bolder: 31-33.
Levin, S. M., 1995. The Importance of Soft Tissues for Structural Support of the Body. Spine: State of the Art Reviews, Volume 9/Number 2, May
Purslow, P.P., Delage, J.P., 2012. General structure and composition of muscle fasciae. In: Scheilp, R., Findley, T.W., Chaitow, C., Huiling, P.A., Fascia: the tensional network of the human body. Elsevier, Oxford, pp. 5-10.
Schleip, R., 2003a. Fascial Plasticity-A new neurobiological explanation: Part 1. Journal of Bodywork and Movement Therapies. 7(1), 11-19.
Schleip, R., 2003b. Fascial Plasticity-A new neurobiological explanation: Part 2. Journal of Bodywork and Movement Therapies. 7(2), 104-116
Schleip, R., Muller, D.V., 2013. Training principles for fascial connective tissues: Scientific foundation and suggested practical applications. Journal of Bodywork and Movement Therapies. 17, 103-115.
Sharkey, J. 2008. Concise Book of Neuromuscular Therapy: A Trigger Point Manual. Chichester, UK: Lotus Publishing. USA: North Atlantic Books, California.
Sharkey, J. 2012. Photo
Sharkey, J. 2013. Photo
Standring, S., (2008). Gray’s Anatomy, The Anatomical Bases of Clinical Practice. (40th ed.). Edinburgh, United Kingdom: Elsevier Churchill Livingston.
Stecco, C., Gagey, O., Belloni, A., 2007b. Anatomy of the deep fascia of the upper limb. Second part: study of innervations. Morphologie, 91, 38-43.
Stecco, A., Macchi, V., Stecco, C. Porzionato, A., Day, J.A., Delmas, V., De Caro, R., 2008. Anatomical study of myofascial continuity in the anterior region of the upper limb. Journal of Movement and Bodywork Therapies. 13(1). 53-62.
Van der Wal, J., 2009. The architecture of the connective tissue in the musculoskeletal system- an often overlooked functional parameters as to proprioception in the locomotor apparatus. International Journal of Therapeutic Massage and Bodywork. 2(4), 9-23.
About the author
 John Sharkey MSc is a Clinical Anatomist, Exercise Physiologist, author and founding member of the BioTensegrity Interest Group (B.I.G.). John is a popular international presentor on topics of bodywork (Medical Massage) and movement therapies. He is a member of the editorial team of the Journal of Bodywork and Movement Therapies and International Journal of Therapeutic Massage & Bodywork and a reviewer for the International Journal of Osteopathic Medicine. John also provides short courses in human anatomy, Thiel soft fix and fresh frozen cadaver dissection with a special focus on BioTensegrity. Visit John’s web site at: www.johnsharkeyevents.com
John Sharkey MSc is a Clinical Anatomist, Exercise Physiologist, author and founding member of the BioTensegrity Interest Group (B.I.G.). John is a popular international presentor on topics of bodywork (Medical Massage) and movement therapies. He is a member of the editorial team of the Journal of Bodywork and Movement Therapies and International Journal of Therapeutic Massage & Bodywork and a reviewer for the International Journal of Osteopathic Medicine. John also provides short courses in human anatomy, Thiel soft fix and fresh frozen cadaver dissection with a special focus on BioTensegrity. Visit John’s web site at: www.johnsharkeyevents.com
Category: Medical Massage
