By Dr. Ross Turchaninov
The article in the July/August issue of Massage&Bodywork Magazine written by Til Luchau is about iliopsoas’ anatomy, role and treatment options. The issue of iliopsoas therapy requires a separate discussion since it is greatly misrepresented and unfortunately misused, especially among massage therapists. This is why we can’t stay away from this extremely important topic.
From the very beginning, the author acknowledges the controversy about iliopsoas’s role and what is more important, about the treatment which is commonly used. Here are quotes from the article:
“…is also clear: direct myofascial work with the psoas is itself controversial”
and even more striking:
“…the potential for client injury (bold by JMS) from intense abdominal work is real”
However, despite the controversy and even blunt acknowledgment that the client can be injured, the author continues to suggest direct intra-abdominal treatment of the iliopsoas muscle. According to the article, the author based his views on:
“…my in-depth readings and study of many others’ reports, opinions and approaches.”
Now let’s see what the author and “others” (BTW we would like to see references of ‘others’) missed during in-depth reading. We will use pictures from the Internet which are very close to the pictures in the article. In the article the author recommends to therapists to (see Fig.1):
“…gently with your client’s breath… sink into the client’s abdomen, patiently making your way to the bottom toward the back and the center (bold by JMS. We will refer to these recommendations later in the review) of the body.”
While doing all of that, the author would like readers to imagine viscera (i.e., omentum, intestinal loops and mesentery) as balloons that will gently slip away, letting the therapist
unobstructively touch the psoas muscle and work with it directly while happy viscera are patiently waiting until the important work is finished.

Fig. 1. The initial position of hands for direct intra-abdominal work on the iliopsoas muscle recommended in the article
For the second part of the ‘therapy’, the article suggests application of the same pressure while the client slowly slides leg up and down along the table as it is shown in Fig. 2.

Fig. 2. Active contraction of iliopsoas muscle while the therapist maintains the intra-abdominal pressure
Arrow – directions of leg movements to activate right iliopsoas muscle
Now let’s see what has actually happened in the abdomen while such ‘therapy’ is performed. First of all as the readers know, the psoas muscle is located so deep that it forms the posterior abdominal wall. Thus all our abdominal organs are located and relying on both psoas muscles as support structures.
Fig. 3 below illustrates the anterior view of the abdomen after the skin and abdominal muscles are removed. As you see, directly under the peritoneum is the omentum, which is an apron shaped connective tissue structure that contains a great amount of fat and it acts as an intestinal protector against any direct abdominal trauma. The omentum has a rich blood supply.
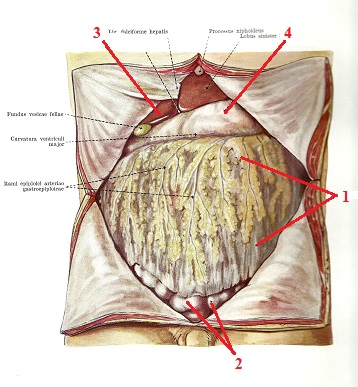
Fig. 3. Anterior view of the abdomen after skin and abdominal muscles are removed
(Kiss and Szentagothai, 1960)
1 – omentum 3 – liver with gallbladder
2 – intestinal loops 4 – stomach
Let’s now remove the omentum (see Fig. 4). Readers can see loops of small intestine as well as large intestine and on the right side red dashed lines indicate lateral and medial edges of the right psoas muscle located under the intestine.
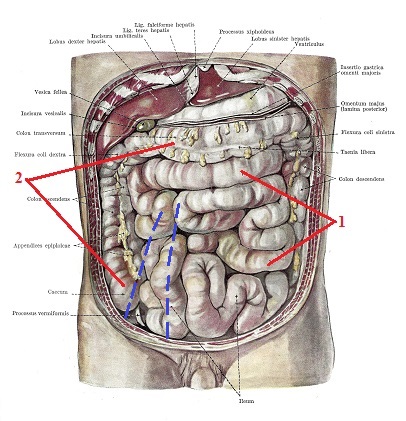
Fig. 4. Anterior view of the abdomen after the omentum is removed
(Kiss and Szentagothai, 1960)
1 – small intestine
2 – large intestine
Blue dashed lines – edges of the right iliopsoas muscle
Our next step is removing the loops of small intestine (see Fig. 5) and now readers may observe the visible fascial fibers which cover the right psoas muscle. We emphasized the borders of the muscle with blue lines. As you can see, the psoas muscle continues under the ascending colon and cecum (blue dashed lines).
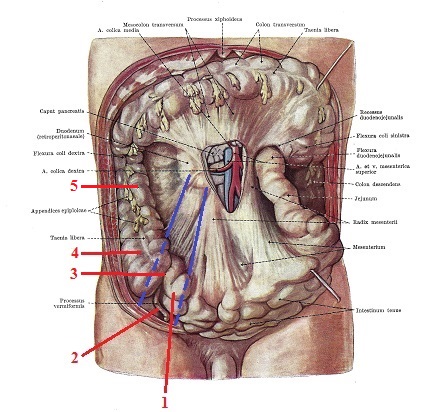
Fig. 5. Abdominal cavity with small intestine removed
(Kiss and Szentagothai, 1960)
1 – jejunum 4 – cecum
2 – appendix 5 – ascending colon
3 – ileocecal area
Blue lines – borders of right psoas muscle
In the left lower corner of the picture you’ll see the ileocecal junction where the ileocecal valve is located. Here the small intestine transitions into the large intestine and the ileocecal valve prevents the intestinal content from moving back into the small intestine.
For the valve to work properly, the cecum and end of jejunum must be stable. This is why this part of the intestinal tract has a very short mesentery and very low mobility. As you can also see, the ileocecal part of the GI lays directly on the right psoas muscle (dashed blue lines).
This is a critical mistake the author, other educators and therapists make. Following the recommendations from the article, the therapist would pin down the ileocecal part of the GI, including the valve against the psoas muscle, at least bruising the intestinal walls and in some cases severely traumatizing them.
Let’s finally remove the large intestine and only now can we see both the psoas muscles and the neighboring anatomical structures (see Fig. 6). Please notice how many layers of abdominal structures must be removed before the therapist can finally get in direct contact with the psoas muscle!
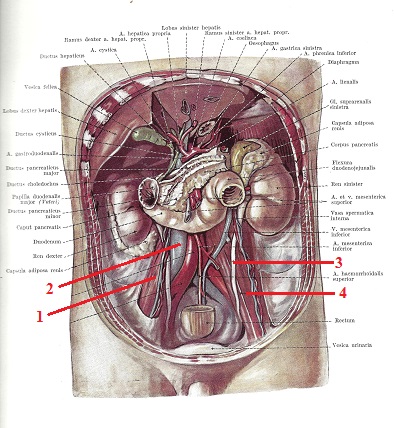
Fig. 6. Posterior abdominal wall with both iliopsoas muscles
(Kiss and Szentagothai, 1960)
1 – right psoas muscle 3 – left ureter
2 – vena cava inverior 4 – left psoas muscle
Please pay attention to the left side where the left ureter crosses the anterior surface of the left psoas muscle exactly where the article suggests therapists work and also notice that the vena cava inferior is normally shifted to the right and it is partly located on the anterior surface of the right psoas muscle.
The notion that while gently sinking into the abdomen, the viscera peacefully slips away exposing the iliopsoas muscle is absurd. The omentum, intestinal loops and/or mesentery don’t
have anywhere to go to escape direct intra-abdominal submergence.
It doesn’t matter what the author thinks, but he will pin down these structures against the psoas and the traumatic impact will increase greatly when the therapist asks the client to slide his or her leg up and down the table.
In such case as a result of contraction of the iliopsoas, the abdominal organs will be additionally compressed and traumatized between the author’s fingertips and the contracting iliopsoas muscle. Should we also mention the left ureter which is on the anterior surface of the psoas muscle and what will happen to it when therapist works on the left psoas muscle?
Of course, the author and “other” unnamed sources have never observed or conducted abdominal surgery. Let us share with the author and readers our personal experience. First of all, the intestinal peristalsis never stops and it is a very gentle process. The video below illustrates the waves of intestinal peristalsis with their sounds recorded during endoscopic laparoscopy.
Are we really reaching the psoas? | By Physio Network | Facebook
The intestinal walls are very gentle, sensitive and easy to damage. This is why when a surgeon touches the intestine to work with it he or she always uses gauze (see Fig. 7).

Fig. 7. The surgeon’s right hand holds intestinal loop with gauze
If the surgeon simply squeezes the intestinal loop he or she holds, it immediately stops its peristaltic waves. As soon as pressure is eased the peristalsis restarts again. This is why young surgeons are constantly reminded by their teachers not to bruise intestinal walls. Imagine for a second what damage to the local peristalsis the therapy suggested in the article does! The direct trauma to the intestinal loop can cause severe consequences in the intestinal function as colitis, invagination, etc. appear later.
One of the main arguments the author uses is gentle pressure during the therapy. However, the pictures in the article show significant submergence into the abdomen, which is accompanied by hand movement and it becomes even more aggressive when the patient starts to move his lower extremity while pressure is still maintained.
The funny thing about all of this is that the author himself is not 100% sure his recommendations will never hurt the patient. Here is a quote from his article:
“This (i.e., iliopsoas treatment by JMS) … is unlikely (bold by JMS) to damage or disrupt the surrounding structures.”
Since the author uses the word “unlikely,” it is obvious that he does not want to 100% guarantee the safety of the therapy. If there is a 1% chance that massage therapy can worsen the patient’s health – and in the case of Mr. Luchau’s recommendations this chance rises dramatically – the author does not have the moral right to promote such ‘therapy’ among practitioners.
Unfortunately the reality of the recommended therapy is much grimmer than the author imagines. The intestine can be easily damaged even by a very small trauma. For example, a simple fall from a bicycle without any other significant trauma (Vijayan and Toe, 2013) or even a
minor collision during a soccer game (Sandiford et al., 2006) can perforate or transect the intestinal walls. These are just two examples from similar publications on this subject in medical literature. Fig. 8 illustrates a complete tear of the intestine observed during surgery after relatively mild trauma.
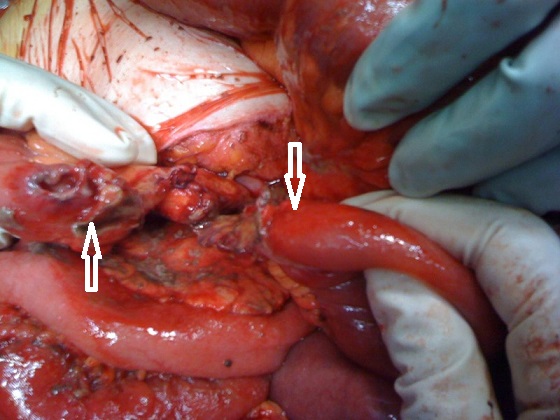
Fig. 8. Jejunal transection after minor external abdominal trauma as it was seen during the
surgery (Vijayan and Toe (2013). The white two arrows indicate both ends of severed jejunum
Vijayan and Toe (2013) concluded that in the reported case the “jejunal transection, presumably by direct compression against the lumbar spine.” We mentioned above in the author’s guidelines about submergence into the abdomen “patiently making your way to the bottom… toward the back and the center of the body.”
Thus the article directs therapists to compress the intestinal loops against the psoas muscle and it is indicated by the words “toward the back” and after that the article recommends switching the direction of pressure “to the center of the body,” compressing intestinal loops and the psoas muscle against the lumbar spine. Thus this is exactly the mechanism of compression described by Vijayan and Toe (2013)!
We would like to emphasize that the clinical cases described above (Sandiford et al., 2006; Vijayan and Toe 2013) occurred when the abdominal muscles were able to protect the intestine since they will always react before any impact reaches the abdominal organs. In the article, the author insists on abdominal breathing and relaxation to remove the abdominal muscles’ protection which will intensify the intestinal trauma.
Of course we are not saying that every treatment promoted in the article ends with perforation of the intestinal loops. However, we guarantee that therapists who follow these recommendations are bruising and traumatizing the lower GI tract. The more therapists follow this absurd procedure, the more chances that one day a therapist will indeed perforate the intestine.
We have always been puzzled where this intra-abdominal psoas treatment came from. Who was that original “genius” who came up with this absurd idea? Our research and communications with other equally surprised somatic practitioners revealed that J. Travel and D. Simmons’s textbook Trigger Point Manual (1983) is to blame.
Technically speaking, it isn’t the book or its authors but an incorrect interpretation of information from it. In Volume II of Trigger Point Manual in the chapter dedicated to the Iliopsoas muscle, Dr. Travel and Dr. Simmons indeed showed the examination of the tension in the iliopsoas muscle (see Fig. 9). In the same way many educators commonly suggest massage therapists actively treat the psoas tension.
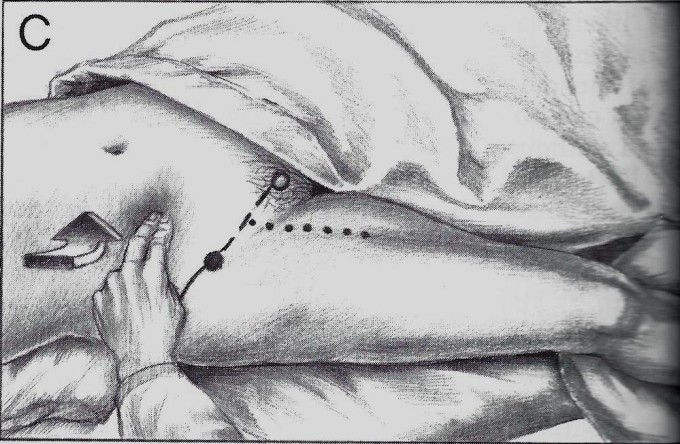
Fig. 9. Examination of the right Iliopsoas Muscle (Travel and Simmons, 1983)
Travel and Simmons showed the correct examination procedure of iliopsoas tension, but it was never intended as a treatment! There is no mention of direct abdominal compression
as a treatment option in their textbook. Somehow this legitimate diagnostic test became a treatment procedure, despite the pure absurdity of this idea.
There is no doubt that direct work with psoas will be helpful for psoas. However if basic rule of medicine: “Do No Harm!” is still relevant for massage therapists the view Mr. Luchau’s approach is unacceptable and his statement,
“Advanced Myofascial Techniques trainings…we see clear benefits that are not easily accomplished by other means”
is an educational disaster.
As long as massage therapy as a profession continues to live in the bubble of unscientific claims (like this one) which are far away from medical science, while whining that no one in the traditional medicine would like to listen – nobody will listen!
There are other means to reduce tension in the iliopsoas muscle which are equally effective. There is a direct approach to the iliopsoas muscle above and below the inguinal ligament completely away from the abdominal organs and direct work on the iliac portion of the iliopsoas when the patient is positioned on the side. There are also indirect therapies like Postisometric Muscular Relaxation. The combination of these approaches gives the same results without injuring the omentum, intestine or mesentery.
Massage therapy is a relatively safe treatment option with few side effects. Direct intra-abdominal work on the iliopsoas muscle is one of the instances when therapists are hurting patients. The intestinal damage can be acute but the pathological changes in the function of the lower GI may also occur later in life following the ‘healing’ effect of intra-abdominal work.
Massage therapy is very flexible in its application. One therapist prefers to use Neuromuscular Therapy while another uses Myofascial Release. In the case of direct treatment of the iliopsoas muscle, there is no compromise since the patient’s health is at stake. Don’t listen to anyone who tells you that iliopsoas must be treated through the abdominal organs! From a medical point of view, this is completely absurd!
REFERENCES
Kiss F., Szentagothai J. Atlas Anatomiae Corporis Humani, Medicina, Budapest, 1960
Sandiford NA, Sutcliffe RP, Khawaja HT. Jejunal transection after blunt abdominal trauma: a report of two cases. Emerg Med J 2006;23:e55
Travel J. G., Simmons D.G. Myofascial Pain and Dysfunction. The Trigger Point Manual. Williams & Wilkins, Baltimore, 1983
Vijayan R, Toe K. Delayed complete small-bowel and mesenteric transection following seemingly minor blunt abdominal trauma BMJ Case Rep. 2013 Mar 8;2013.
Category: Medical Massage
Tags: Issue #4 2015
