By Dr. Ross Turchaninov, Phoenix, AZ
Our clinic has a limited number of regular patients since we do whatever it takes to completely fix the problem and give patients enough home tools to prevent the same symptoms from coming back. However, we do have some patients who we see regularly: every month, every couple weeks or even every week. The main reason for that is the advanced stages of abnormalities they suffer from and those patients require maintenance.
Here is a recent case of one of our regular patients who comes to the clinic every Thursday since she has a very advanced case of Fibromyalgia (FM). Our weekly sessions allow her to have a normal, productive life.
Several weeks ago, she came in for her weekly session and mentioned that she recently developed pain in her left elbow, which was getting progressively worse. She visited her rheumatologist who diagnosed her with Acute Tennis Elbow. Her physician also offered her a steroid injection to decrease local inflammation in the area of the lateral epicondyle. She decided to consult our clinic first.
EVALUATION
Evaluation of the patient’s elbow indeed confirmed a clinical picture of acute Tennis Elbow: pain in the lateral elbow when the patient makes a fist. She reported acute pain when direct compression was applied to the periosteum of the lateral epicondyle and to the tendinous part of the hand extensors. There were not any signs of radial nerve compression.
TREATMENT
Since she has very active FM there is no way we can use any aggressive Medical Massage techniques. For this reason, the therapy would be longer than usual. We informed her about it and she agreed. We also suggested to her that after we removed the initial protective muscle tension from the extensors, she may consider steroid injection as an additional treatment tool. Otherwise the presence of FM may significantly prolong therapy.
1st session
During the first session we concentrated on the lymph drainage and on decreasing protective muscle tension in the extensors on the dorsal surface of the forearm. We agreed with the patient to conduct the next session on an upcoming Monday.
2nd session
As soon as the patient got to the therapy room she was visually upset since according to her she developed a skin allergic reaction to the oil after the first session. It was very puzzling since the oil we used was the same oil we use on her weekly.
As soon the patient showed her forearm it was obvious that the rheumatologist as well as we made a mistake and the patient didn’t have Tennis Elbow but an acute attack of Shingles. Fig. 1 shows the patient’s forearm at the beginning of the second session.
Fig. 1. The patient’s forearm at the beginning of the second session
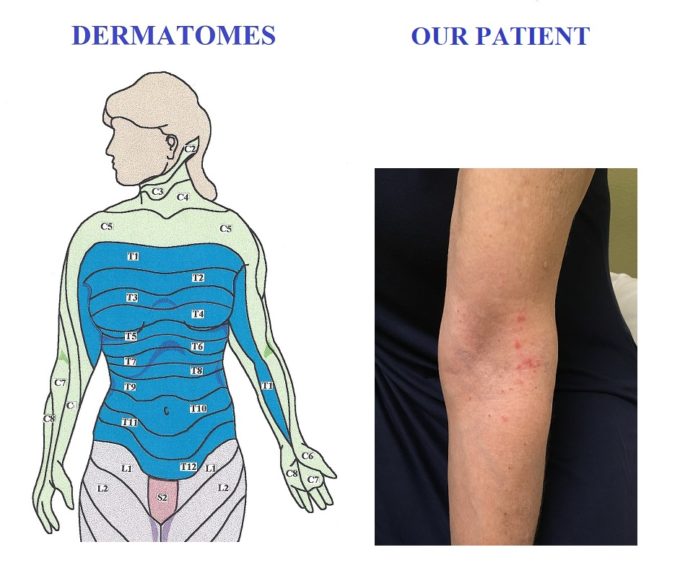
As you can see, the skin lesions caused by herpes virus have a very distinctive appearance. They are red pimples with clear vesicle on the top and they always follow the direction of the dermatomes. Fig. 2 compares the location of the patient’s lesions and orientation of the dermatomes on the left arm and forearm.
Fig. 2. Comparison of our patient’s lesions and map of dermatomes
As you may see on the picture above her C5 dermatome affected and the lesions are arranged vertically along the vertically oriented dermatome. If Shingles were located on the chest, the lesions would be oriented horizontally, since dermatomes on the trunk run in perpendicular direction to the vertical axis of the body (see orientation of trunk dermatomes in Fig. 2).
Shingles is a result of chronic infection by herpes virus. After initial exposure to the virus it settles within the spinal of peripheral nerves and it can be easily reactivated by emotional or physical stress, exposure to lower temperature, other infections etc., i.e., all factors which may weaken the immune system. As soon as the virus finds gaps within the immune system’s defense it starts to multiply within the affected nerves triggering local inflammation. This inflammation causes nerves to swell but initially it manifests itself as different patterns of somatic or visceral pain without any other symptoms.
In the case of our patient it was a clinical picture of Tennis Elbow. Very frequently Shingles on the left side of the chest manifests itself as symptoms of heart attack and so on. If Shingles happened one time there is great chance that it will strike again in the same exact spot or it can be a completely new area of the body. Previously our patient had Shingles on her chest once and this attack was the second episode but she didn’t correlate them as a manifestation of the same problem.
While the virus continues to multiply and move along the nerve, the only symptom the patient continues to have is acute pain. When the virus reaches the end of the nerve it manifests itself as skin lesions along the dermatome supplied by the nerve and only at this point the real cause of the clinical picture became obvious.
The most confusing part of Shingles is that very frequently there is a significant time lapse between onset of the pain and formation of skin lesions. In the case of our patient, skin lesions appeared almost two weeks after the onset of the pain.
The only solution for such a situation is immediate referral of the patient to a primary care physician who will place the patient on anti-viral medications and if there are a lot of lesions oral steroids also be required to decrease inflammation within the nerve and prevent its damage. The anti-viral therapy eliminated our patient’s elbow pain in 3 days.
LESSONS:
1. Always pay attention and examine the patient’s skin. In the past several years we have observed a significant increase in the number of patients with Shingles, which initially shows itself as pure somatic or even visceral pain in different locations.
2. In our clinic we observed several patients who exhibited Shingles as a single skin lesion. Such cases were very rare occasions before. So be observant!
3. The patients with chronic Shingles which attacks the same area always exhibit skin discolorations and even scarifications. If this is the case you will see dark pigmentations in the areas of recurrent skin lesions.
Fig. 3 illustrates another patient with Shingles from our clinic who suffered for years from lower back pain but no one actually examined her gluteal area and sacrum since she always thought that these pimples are allergy reaction. As you see in the picture below, the scarifications from previous outbreaks are clearly visible.
Fig. 3. Skin of the patient with chronic Shingles infection
4. Don’t treat the patient until even residuals of skin lesions are cleared up. After that you may access the clinical symptoms since some patients may exhibit secondary sensory abnormalities in the form of tingling, burning or itching. If these symptoms are present the therapist is supposed to work in affected areas resetting the normal threshold of sensory receptors.
Category: Blog