By Dr. Ross Turchaninov,
Phoenix, AZ
In this clinical case we are going to illustrate one important notion: Medical Massage practice is an essential part of the MT profession and medicine in general since it delivers stable clinical results even in very complex cases.
The patient is a 55 year-old female who works as a hairdresser. For years she experienced chronic lower back pain in part due to her long working hours. Several years ago, a lower back MRI confirmed the presence of posterior 5 mm L5 disk herniation with spinal canal stenosis.
During the last 5 years she was periodically seen in our clinic (1-2 times per year) with moderate and rarely acute lower back pain which we were able to successfully control while she did her regular maintenance at home.
Her hair salon was closed due to the coronavirus pandemic. Just before Easter she decided to clean her entire house including the backyard and she did it in one day. The next day she woke up with screaming pain and the complete inability to move due to the pain and her right leg weakness. The pain was radiating all way to both legs especially to her right foot, making it completely numb and putting her entire lower extremity on ‘fire’.
Patient’s husband called 911 and an ambulance delivered her to the nearest emergency room. An MRI was performed which confirmed the presence of central L4-L5 disk extrusion with severe central canal spinal stenosis and bi-lateral foraminal stenosis. In other words the content of her disk leaked out posteriorly and dramatically decreased space for the spinal canal and both foramens which let L5 spinal nerves out of vertebral column. Fig. 1 illustrates the radiologist’s report.
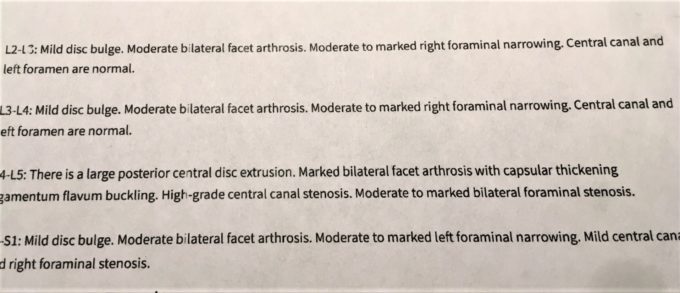
Fig. 1. Patient’s radiologist report from the emergency room
Due to severe pain the epidural injection was performed in the hospital and she was released home with recommendations to see a neurologist and/or neurosurgeon. She was also given a prescription for pain medication, muscle relaxant and gabapentin (to decrease spinal nerve inflammation).
The next day after her epidural injection she got some relief in the intensity of her symptoms. She waited three more days, but there wasn’t any further improvement. She consulted a neurologist and he suggested she see a neurosurgeon. Considering that she was successfully treated in our clinic, the patient made an appointment as soon as she was able to move independently.
The video below illustrates her walking to the therapy room in the corridor of our clinic. At the moment the video was taken she already had one epidural injection and she was on heavy medications. That is how disk extrusion looks clinically.
EVALUATION
The patient was pale, breathing superficially and frequently (tachypnea), sweating profusely, her blood pressure was 160/90, and most of the time she felt nauseous. All of that indicated that the spinal nerve’s compression triggered a protective reaction in form of lower back acute pain which in turn greatly disbalanced her autonomic nervous system, initiating severe autonomic reactions from various system and organs.
There is no way to examine anything since the patient was still in screaming pain while getting on the table.
TREATMENT
The first two sessions were used to inhibit the pain analyzing system and decrease protective muscle tension. We concentrated on the middle back, sacrum and finally lumbar area. We used LDM in combination with an inhibitory regime of massage therapy, careful application of relaxation of the paravertebral muscles techniques, permanent electric vibration, activation of H-reflex and gentle passive stretchings. She was given homework supportive recommendations and she must to do light exercise in the swimming pool.
By the third session the patient was still in acute pain, but she was able to get around easier and she was standing straighter. She felt great pain relief while she was in the water and pain came back as soon she got out of the pool.
At that time, it became possible to examine her soft tissues. As we predicted her lumbodorsal fascia exhibited severe shortening including its insertions to SI joints, periosteum of the sacrum and lateral surfaces of lumbar spinous processes. The Sensory Test indicated sensory deficit along L4-L5 dermatomes due to the cutaneous branches being compressed by the lumbodorsal fascia and lumbar erectors; abandoned active TPs were detected in lumbar erectors and quadratus lumborum muscles; periostal changes in the spinous processes of lumbar vertebrae, entire right side of sacrum and right SI joint and iliac crest all way to its middle point.
Thus 3-7 sessions were dedicated to usage of soft tissue rehabilitation modalities to decompress the entire lower back and finally L4-L5 segment specifically.
To do that we gradually added Connective Tissue Massage with elements of Myofascial Release, Trigger Point Therapy, Postisometric Muscular Relaxation and decompression of periosteum using Cyriax’s friction and Periostal Massage.
The video below illustrates our patient walking in the clinic corridor after the 10th session of Medical Massage protocol for Lumbalgia. What separates the first and second video are 10 every other day sessions of Medical Massage.
The patient was advised to re-start inversion table usage, continue to do home routine and water exercise. She is not on any medication anymore and she experienced only morning stiffness in the lower back which she was able to control. The patient is not unique for our clinic. We deal with similar patients on a daily basis. Thus, Medical Massage therapy IS essential business for our patients and patients our students are working with.
LESSONS:
- The patient had a very severe clinical case. Even after epidural injection in the emergency room the only solution offered to her was spinal surgery. There are no doubts that the patient suffered from severe disk pathology and disk extrusion is the most advanced deterioration. Her disk extruded into spinal canal and pinched both spinal nerves. However, it’s always worth a try to decompress the soft tissue component of the affected vertebral segment by Medical Massage first. If Medical Massage fails, the option of surgery is always still available.
- Why did such relatively simple therapy, compared to the complexity of the spinal surgery, eliminate the need for surgical intervention? The first clue that conservative therapy, in the form of Medical Massage, may work for this patient was the significant reduction of the symptom’s intensity in the water. Secondly, layer by layer decompression of the soft tissues in the lower and middle back eventually decreased pressure within spinal canal and created extra space for the L5 spinal nerves to function and eventually eliminated clinical symptoms.
- Were the results which were presented in the second video long lasting? Yes, if the patient is committed to do her homework regularly and comes to the clinic for supportive therapy every month the pain free function is more likely sustained. Due to the natural process of aging her disks are going to dry out, triggering so called ‘natural fusion’ and she is supposed to be completely pain free while some ROM of course is going to be lost. However, it is a small price to pay compared to the 30% failure rate of spinal surgeries.
- The recent pandemic has greatly affected the entire country, including the MT profession. In many states MT is considered a non-essential business and its practice is forbidden to prevent the spread of the virus. There are a number of educators and therapists who correctly supported shutting down clinics on the basis that these services are non-essential. There is no doubt that it is absolutely ridiculous and unprofessional to practice pregnancy massage, oncology massage or even stress reducing massage while the therapist and client can be potentially exposed to the virus. In our clinic we also cancelled all supportive therapies.
- However, let’s look at that situation our patient was in when she entered our clinic after her first epidural injection. She was still in an enormous amount of pain and dysfunction and her treatment options were greatly limited since even spinal surgery was out of question since hospitals at that time cancelled all surgical procedures except emergencies. Our point is that in emergency situations, similar to what we described, Medical Massage IS the essential medical procedure and patients must have access to it the same way as they have it with DC or PT offices. Of course, with all possible precautions. Our clinic deals weekly with patients who suffer from clinical picture of similar intensity and we simply unable to say them ‘NO’ and suggest waiting for another month or two.
Successful treatment of this and similarly complex cases was possible only because of the clinical power of Medical Massage. The science-based Medical Massage Theory is information of such importance, that SOMI requires our students to take it twice during our Medical Massage Certification. While many practices are still restricted we suggest therapists two new online classes which cover the first day of lecture, “Introduction to Medical Massage from Theory to Application.”
Begin your journey into Medical Massage by slowly absorbing this valuable information at your own pace. Both online classes are approved by NCBTMB and accepted by SOMI as part of our Certified Medical Massage Practitioner Program. These classes have been developed by practitioners who were once SOMI students and who recognized the need to provide solid science-based data for you in online format. We can assure therapists of the unprecedented quality of information and we like the friendly way this important data is presented. SOMI does not have financial interest in these projects. Here are links to two on-line classes:
1. By Shea Shulman, CMMP, LMT: https://www.studymedicalmassage.com/
2. By Dr. Jeff Cullers, DC, CMMP, LMT: https://www.premiercontinuingeducation.com/
Category: Blog


