Thank you everybody for the comments left in our FB post. It is great to see active engagement of the therapists who practice clinical aspects of MT. Many causes to the condition initially described in the post were mentioned. Let us summarize them: tension in lumbar erectors, quadratus lumborum, piriformis, iliopsoas, adductors, fascia latae muscles, misalignment of the sacroiliac joint, lumbar disk pathology with radiculopathy etc.
Ironically, all therapists who commented on this clinical situation were correct. Indeed, the patient exhibited all these symptoms. However, they were the brain’s protective reactions to a completely different cause which was missed by different health practitioners who previously worked on this patient. The real cause has hidden behind layers of secondary symptoms which clinically pronounced themselves and hid the real trigger. So those readers who mentioned hip joint pathology were right to the point.
Science Of Massage Institute
MEDICAL MASSAGE VS HIP OSTEOARTHRITIS
by Dr. Ross Turchaninov,
Phoenix, AZ
The patient is a 45 year-old working from home IT specialist. He came to the clinic with complaints of left lower back pain and left lateral and anterior hip pain which radiates to the groin. Pain in the left hip especially sharp when he gets up from the chair or during first steps in the morning. The level of pain decreases with active movements. These symptoms started approximately year ago and slowly got progressively worse.
Initially the patient visited a chiropractor who did his lower back X-Ray and detected the presence of slight right-side Lumbar Scoliosis and narrowing of L4-L5 and L5-S1 intervertebral spaces. The doctor correctly considered this curve to be so-called compensatory scoliosis and diagnosis Degenerative Disease of the Spine was established. After combined therapy by the chiropractor and massage therapist the patient was almost completely pain free for 2-3 weeks, but the same symptoms eventually came back.
The patient went to his PCP with an already established diagnosis and a doctor sent him to physical therapy which again helped him a lot, but the same symptoms eventually came back. He was also treated by an acupuncturist and another massage therapist with similar results.
VISUAL EVALUATION
The patient is moderately overweight, and he slightly limps on the left side when he walks. His foot is in outer rotation (Freiberg’s Sign) which indicates significant tension in piriformis muscle.
TESTING AND PALPATION
The patient exhibited tension in the lower back in superficial fascia, lumbar erectors and quadratus lumborum muscles on both sides, but the degree of tension is more prominent on the left. Active TP was registered in left piriformis muscle.
Various Compression Tests indicated local tension, but they didn’t provoke neurological reactions. The patient never experienced numbness, ‘pins and needles’ sensations on his lower back or left lower extremity.
The palpation of the soft tissues on the lateral and anterior hip and groin immediately triggered withdrawal. The tensor fasciae latae, rectus femoris, iliopsoas and especially adductors harbor active trigger points. The patient also exhibited very active and painful periostal trigger points at the muscles’ insertions into greater trochanter, iliac spine and pubic bone on the left.
Palpation of the anterior hip above and below inguinal ligament is very painful. Examination of ROM indicted restricted abduction and inner rotation in the left hip joint. Fig. 1 illustrates significant restriction of passive abduction in the left hip joint.

Fig. 1. Degree of passive abduction in the left (affected) compared to right (unaffected) hip joint.
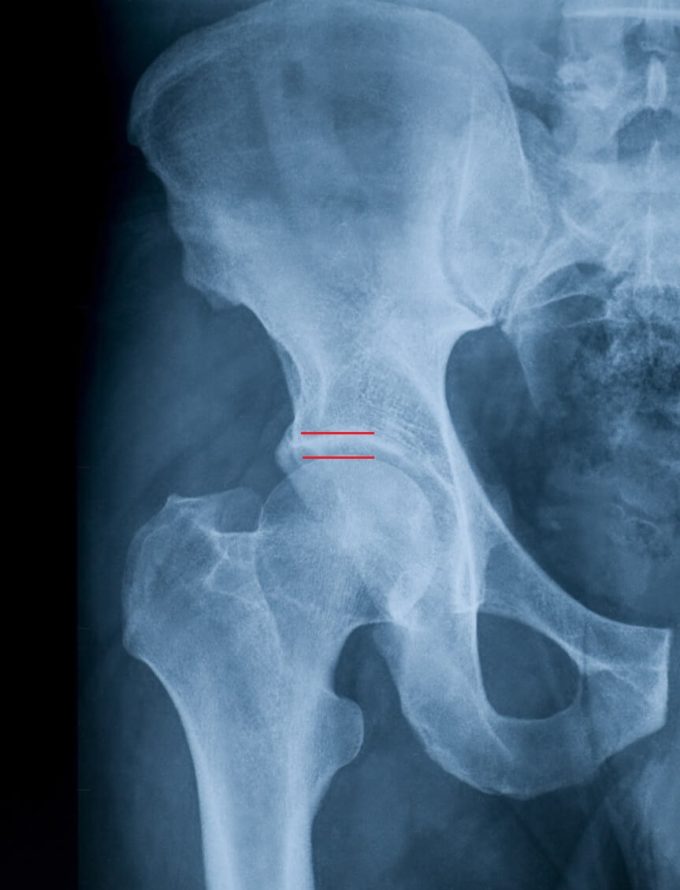
The measurement of the patient’s left lower extremity indicated almost half an inch shortening. Considering the patient was unsuccessfully treated for various pain syndromes in the lower back and pelvis it was obvious there was something else causing his pain and dysfunction. All signs pointed to Hip Osteoarthritis which no one even considered. We suggested the patient see a physician in our clinic who is going to examine his left hip joint. X-ray had indicated moderate Degenerative Joint Disease (OA) of the left hip joint with joint space narrowing and spurs formation inside of the joint (see Fig. 2).
TREATMENT
After the diagnosis of left Hip OA was established, we used full power of Medical Massage protocol for the hip OA. The goals were: decompression of the joint, decrease pressure on already compromised cartilage and slow down or stop further development of OA.
Each session started with addressing the lower back to eliminate pain and dysfunction there and restore correct lower back/pelvis dynamics. However, the main part of the therapy was dedicated to decompression of the left hip joint. The therapy was sequentially targeting soft tissues in the gluteal area, lateral hip (tensor fascia latae muscle with IT band), anterior hip (including iliopsoas muscle) and finally the area of adductors. We combined elements of: Lymph Drainage, Connective Tissue Massage, Neuromuscular Therapy, Trigger Point Therapy, Myofascial Release, Muscle Energy Technique and Periostal Massage.
After soft tissue release in each part of the hip, the joint itself was stretched along the axis of the joint and along the axis of the lower extremity. The patient used supportive therapy at home which included: frequent stretching, hot showers, inversion table and light repetitive exercise in the swimming pool. Fig. 3 illustrates the patient’s hip abduction after 5 sessions of Medical Massage

Fig. 3. Passive hip abduction after 5 sessions of Medical Massage
After 5 sessions the patient didn’t have lower back pain and stopped limping. However, he still experienced moderate discomfort after getting up and at first several steps. We continued the same treatment routine for five more sessions. Fig. 4 illustrates the degree of passive abduction at the end of the therapy. At that time, the patient didn’t exhibit the original clinical symptoms. You may also see that his passive abduction on the left is now greater than on his right non affected side.

Fig. 4. Passive abduction at the end of the course of Medical Massage therapy.
Currently we see the patient once a month for supportive therapy. The same results are maintained for last four months.
DISCUSSION:
1. Let’s go over the clinical reasoning for this patient.
a. No hip trauma. It means that muscle strain (e.g., adductors and iliopsoas muscles) or trauma of the joint itself (e.g., labrum) are out of the potential causes
b. It seemed that the pain did not have neurological origin. It wasn’t diagnosed by his doctors and he didn’t have a history of burning, ‘pins and needles’, numbness. All Compression Tests were negative.
c. The patient’s pain is mostly on the anterior surface of the hip joint and after that it radiates to the groin. The pain is especially acute at the beginning of walking and in the morning. He now constantly limps. Movements decrease pain intensity.
d. The most important sign is restricted abduction and both inner and especially outer rotations in the left hip joint when it was compared to the right. The combination of inner osteophytes (spurs) and the joint space narrowing are frequent hidden cause of such multi-layered somatic pathology.
e. There is expected tension in the lower back due to the limping
All of that indicated that the function of his left hip should be examined. The patient was sent to pelvis and both hips X-ray by our physician and tests confirmed the hip joint degeneration.
2. It is a clinical mistake to concentrate on the lower back, as it was done prior, because the tension there is the result of the protective brain’s reaction to the hip joint’s degeneration. In these patients, the therapist is going to observe different degrees of local tension in the lower back and various postural changes (limp, tilt of the pelvis etc.) which formed secondarily.
3. Let’s restore a logical chain of events. For different reasons the cartilage which covered bones of the left hip joint became thinner. The receptors inside the hip joint informed the brain about cartilage degeneration and the brain took necessary actions. The brain has a limited number of tools to help the suffering joint at this point. To minimize further degeneration of the joint the brain started to alter the patient’s gait, change position of the pelvis, formed compensatory scoliosis etc., without him being aware of it. All these compensatory tools allowed the patent to function for a while on in other words he was in the compensatory stage.
The fact that the patient started to feel pain indicated that these compensatory tools failed, and he entered the decompensation stage. It meant that in some small areas the cartilage was dangerously thin and the subchondral bone (i.e. bone which supports cartilage from under it) was under excessive pressure.
As soon as the subchondral bone came under increased compression force, during even regular walking, the nociceptors (previously known as ‘pain receptors’) became activated and formed the alarming sensory input to the brain. Only at this moment the patient started to FEEL pain in the left hip because sensory cortex formed pain sensation based on the data obtained from nociceptors. At that moment new compensatory reactions (a.k.a. new pain syndromes) developed in the soft issues which participate into hip stabilization and active movements. As a result a multi-layered somatic pathology developing and it additionally clouding an already complex clinical picture. At that moment new compensatory reactions (a.k.a. new pain syndromes) developed in the soft issues which involved into the hip stabilization and active movements forming multi-layered somatic pathology additionally clouding already complex clinical picture.
Since each sensory input to the CNS should produce motor output and the new strategy the brain engaged to help the compromised joint was an initial call the patient made when he contacted his chiropractor. The doctor correctly identified the most obvious components of the clinical picture he observed, but he and other health practitioners were facing the secondary compensatory reactions which were layered on top of each other and they hid the real cause.
3. The legitimate question is how stable the clinical outcomes of Medical Massage are? There is no way Medical Massage as well as any other modality can restore damaged cartilage or remove osteophytes. So, further hip degeneration is expected while the patient is getting older. So why is Medical Massage beneficial for this patient and maybe immediate hip replacement is the ultimate and quicker solution?
The answer to this speculation is quite simple. On average the current age of modern hip endoprosthesis is between 15-20 years. The patient is 45 years old and if hip joint continues to degenerate the early hip replacement surgery is needed. In such case there is very big chance that the patient is going to need another surgery at the age when his health is going to decline due to the normal process of aging and there is a greater chance of further complications after the second surgery (endoprosthesis’ instability, osteoporosis, scar tissue formation etc.).
A proper regime of supportive Medical Massage therapy in combination with other somatic modalities (chiropractic, acupuncture, exercise etc.) and regular homework guarantee that hip replacement surgery can be postponed to the later age and in such case the surgery’s results are going to be clinically stable. There is also a slight chance that the correct management of his hip joint may ‘freeze’ its further deterioration.
LESSONS:
1. Please use the same strategy of analysis in each case of chronic pain and dysfunction because if there is no previous trauma in the history of illness the therapist more likely faces secondarily compensatory reactions which pile on top of the initial trigger.
2. If the patient presents chronic abnormality the pain itself is not pathology but rather a ‘cry for help’ from the patient’s CNS. Do not treat pain – identify and eliminate it at the source!
3. Some therapists mentioned in their comments that our post was inappropriate since we promoted establishing diagnosis which is out of therapists’ scope of practice. That is a very unfortunate and erroneous position which undermines the clinical power of Medical Massage and other somatic manual modalities. It is simply an outdated concept which greatly narrows the therapists performance and undermine vital part of the medicine.
Let’s us give following example, the patient was in car accident, and after that he went to his PCP and a diagnosis of ‘Whiplash’ was established by the doctor. According to ICD-10 medical coding system this diagnosis has s13.4XXA code and the medical office getting paid by the insurance company accordingly. Later, the same patient was referred to the massage therapy or physical therapy clinic and the patient comes there with the same diagnosis. We are curious how the diagnosis “Whiplash’ is going to help the therapist (who is against diagnostic evaluation of the soft tissues) in formulating a correct treatment strategy?
The ‘Whiplash’ diagnosis didn’t specify if trapezius or levator scapulae muscle that were traumatized, if fascia was damaged, if greater occipital nerve is compressed triggering severe headache as a result of whiplash, etc.
Diagnostic evaluation of the soft tissues IS within the scope of practice for those who accumulate enough knowledge and clinical expertise. Daily, our former students conduct diagnostic evaluation of soft tissues while working with physicians and chiropractors who value their professional input. So, don’t diminish the clinical possibilities MT offers to patients, therapists and physicians.
Category: Blog