By Dr. Ross Turchaninov, MD
As discussed in the first part of this article, (Medical Massage Courses & Certification | Science of Massage Institute » PERIOSTAL MASSAGE. PART I: STRUCTURE AND FUNCTIONS OF PERIOSTEUM) the periosteum is the central functioning component of healthy bones that supports our entire skeleton. The periosteum is a part of soft tissues; therefore, medical massage, specifically Periostal Massage, should address its dysfunctions. However, before discussing this vital treatment, we must cover the mechanisms behind periosteal dysfunctions.
Therapists face periosteum pathologies daily without realizing it. Common manifestations include:
Osteoarthritis (early stages); Tennis Elbow; Golfer’s Elbow; Occipital Headache; De Quervain’s Disease; Radial Styloiditis; Various Rib Dysfunctions, Trochanteritis, Inflammation of sacroiliac joints (Sacroiliitis), Leg Compartment Syndromes; Periostitis of the Heel Bone; Calcaneal Spur, etc.
These abnormalities trigger pain and dysfunction and are frequently treated as something else. For example, a patient may complain of cramps and active trigger points in the gastrocnemius muscle. In reality, these symptoms are formed secondarily as a reaction to the periosteal inflammation at the Achilles tendon insertion into the heel bone or due to inflammation at the insertions of superficial and deep fascia to the tibia. Therefore, understanding the nature of periosteal dysfunction is so important. There are three leading causes of periosteal dysfunction: trauma, chronic tension in the soft tissues, and reflex zone formation.
Trauma
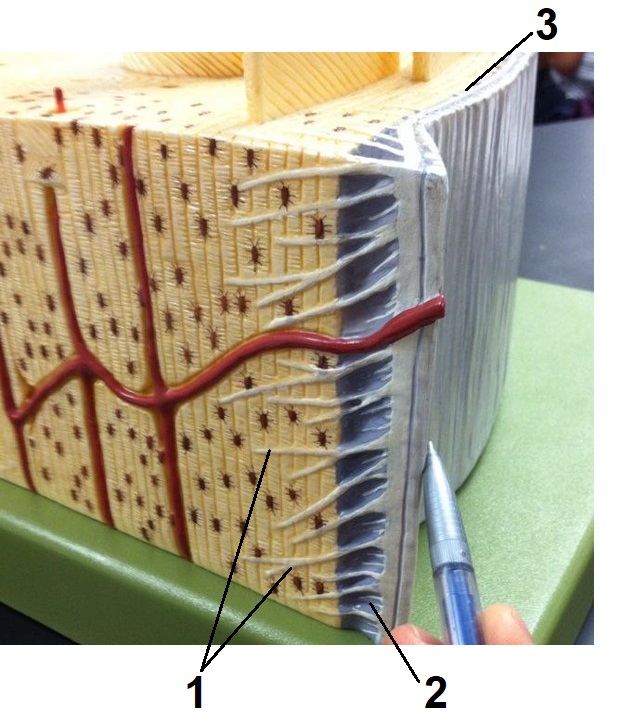
If the patient lifted underestimated weight or had direct trauma, the applied forces may exceed the stability of the periosteum at the tendon or ligament insertions. As a result, the periosteum is slightly pulled off or even detached from the underlying bone (depending on the power of contractile force). In such cases, Sharpey’s fibers grown into the bone to stabilize the periosteum are entirely or partly damaged (see Fig. 1).
The first part of this article explains that the periosteum is richly innervated. When the periosteum becomes inflamed, even mild muscle contraction jerk the affected periosteum creating much discomfort and acute pain. The pain may be so severe that a patient with Tennis Elbow, for example, can’t even hold a cup of coffee in their hand. Fig. 1 illustrates the detachment of the periosteum from the bone due to excessive force elicited by contracted muscles.
1 – strained and damaged Sharpey’s fibers
2 – detached periosteum
3 – normally attached periosteum
Chronic Tension In Soft Tissues
Work requiring repetitive motions or excessive exercise in the gym may trigger different forms of periosteal dysfunction. For instance, squeezing the handles of the elliptical machine while doing a cardiovascular workout for 40-60 minutes may trigger Golfer’s, Tennis Elbow, or De Quervain’s Disease. In these cases, steady pressure elicited by the tendons and ligaments at their insertions into the periosteum cause irritation. Despite mild irritation, the local inflammation and acute pain are triggered even without periosteum detachment.
Periosteal Reflex Zones (PRZs)
PRZs have much less exposure than the previously discussed causes of periosteal dysfunction. However, in clinical reality, PRZs is a vital issue as therapists face them daily.
Like every organ and tissue, the periosteum requires proper oxygenation through the circulation to function. Some organs require a lot of oxygen, and circulation is abundant (e.g., the brain). Others, like the peripheral nerves, can’t have direct blood flow since any fluid inside the nerve will block the conductance of electrical impulses (i.e., action potentials).
The periosteum supports blood circulation in the bones by letting the arteries and veins pass through the inner layer of the periosteum. As we discussed in the previous article, the osteoblasts are located in the inner layer of the periosteum, and this part of the periosteum is highly vascularized. However, the outer layer of the periosteum consisting of dense connective tissue, is poorly vascularized. Vascularization for the outer layer is sacrificed for the periosteum’s stability at its insertions into the bone. If the outer layer of the periosteum is highly vascularized, it becomes weaker and cannot stabilize the soft tissues.
In such a case, there is the legitimate question of how the outer layer of the periosteum ‘breathes,’, especially under such tremendous pressure elicited by contracting muscles. The outer periosteum ‘breathes’ by a so-called diffusion process. More oxygenated blood AROUND periosteum, more oxygen enters it.
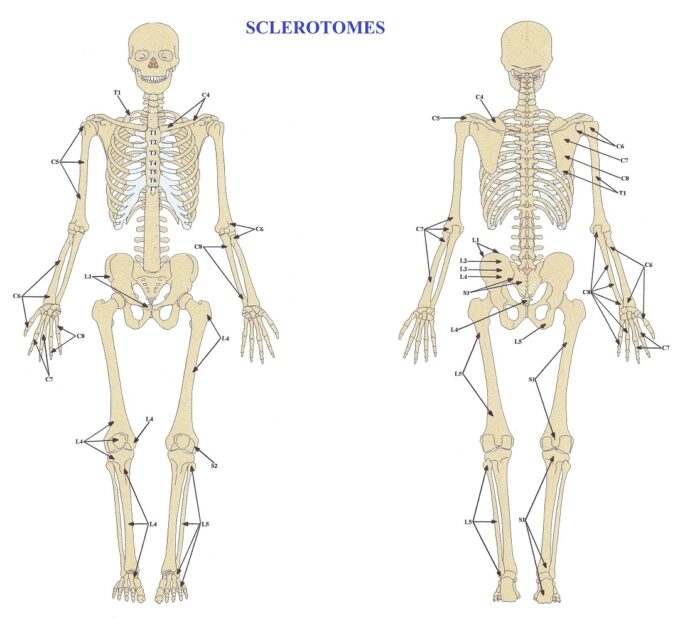
Different parts of the periosteum, similar to the skin, are innervated by different spinal cord segments. The pattern of the periosteum’s innervation is called the Map of Sclerotomes (Fig. 2).
The topic of sclerotomes brings us closer to the concept of reflex zones which are discussed in a separate article:
Let’s discuss the clinical value of oxygenation and innervation of the periosteum on the example of the Tennis Elbow. Yes, inflammation of the lateral epicondyle of the humerus can result from direct trauma or chronic tension in the soft tissues due to steady muscle contraction. However, in many cases of Tennis Elbow, the initial cause of the periosteum’s inflammation and/or detachment is the presence of periosteal reflex zones. In these cases, the chronic, minor irritation of the radial nerve by other somatic pathologies makes the periosteum of the lateral epicondyle weaker, and it is easier to traumatize it. In these cases, all local treatments used to restore the proper functioning of the periosteum are useless because the silent trigger is in a completely different body part.
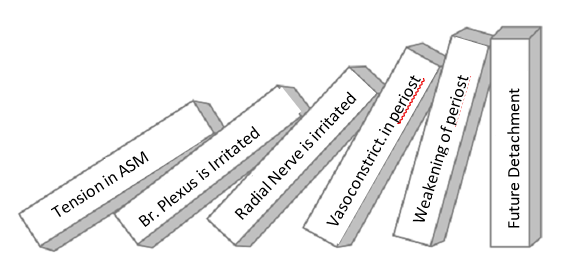
The ‘domino effect’ governs every chronic pathology in the human body. While abnormality continues to progress, different domino pieces start to collapse, and the therapist must understand the process to be clinically effective. Understanding this process is key to learning gained through Medical Massage Training by the Science of Massage Institute.
Let’s discuss the ‘domino effect in the example of tension in the anterior neck that triggers the Tennis Elbow. By recreating the chain of events, we know that the tensed anterior scalene muscle on the anterior neck may slightly irritate part of the brachial plexus that gives origin to the radial nerve, which later innervates the lateral epicondyle. When nerve irritation is mild, the patient doesn’t experience discomfort in the anterior neck. Their complaints are instead related only to the lateral epicondyle, where the fibers of the irritated radial nerve end. Please view the diagram in Fig. 3
Local vasoconstriction in the soft tissues is the first consequence of radial nerve irritation. However, even a completely healthy elbow has lower circulation in the periosteum of the lateral epicondyle. Therefore, when less oxygen comes to the surrounding tissues, the diffusion process that the periosteum uses to breathe is blocked. When oxygenation of the periosteum diminishes, it weakens its attachment to the underlying bone (tears of Sharpey’s fibers shown in Fig.1). The periosteum can no longer resist the force elicited by powerfully contracting muscles, and it gets inflamed and/or detached from the periosteum triggering Tennis Elbow.
Suppose the therapist treats Tennis Elbow using local therapy (as is frequently suggested) and ignores PRZs formation. In doing so, the therapist will never be able to achieve stable clinical results, and the symptoms of Tennis Elbow will return with the same or even elevated ferocity. Eliminating the initial trigger of the Tennis Elbow before any work on the elbow begins would be the only way to treat the patient’s condition.
In Part III of this article, we will discuss Periosteal Dysfunctions And Their Evaluation.
Please join SOMI on November 12-13 for a Live Webinar (8 CEUs) dedicated to the Theory of Medical Massage and Soft Tissue Evaluation: Medical Massage Courses & Certification | Science of Massage Institute » SOMI’s Webinar November 12-13

Category: Medical Massage
Tags: 2022 Issue #2