Before presenting the clinical case sent to us by our former student, Steve Smith, LMT, CMMP, we would like to share its history. Former and current students of SOMI form a professional network to stimulate mutual growth and provide reciprocal referrals. It helps the patients to expedite finding proper Medical Massage help. Steve’s submission is an excellent example of that.
This case started with a woman experiencing a health challenge who struck up a conversation with a fellow traveler while sitting in an airport. She explained her dire situation, which nobody had resolved, and the woman next to her passionately suggested she contact the Medical Massage Practitioner who helped her with similar swallowing problems. The contact info she provided was for a professional therapist in New Jersey, our former student, Teresa Brumble, LMT, CMMP, whose work indeed specializes in swallowing dysfunction, called Dysphagia. Previously Teresa had had another patient with Dysphagia, and she used treatment from our clinic that we readily share with therapists. (Medical Massage Courses & Certification | Science of Massage Institute » MEDICAL MASSAGE VS SWALLOWING PROBLEM)
After an hour-long consultation, the patient immediately phoned Teresa, who suggested that she contact Steve Smith, also a graduate from SOMI’s Medical Massage Certification program, as he was practicing in the Denver area where she resided. This is how the patient got in touch with Steve, and he solved her complex clinical case, which nobody else could resolve, and gave the patient her life back.
Using the clinical tools SOMI offered, Steve became an independently thinking massage clinician, able to mix skills he’s learned and create unique Medical Massage protocols for his patients. We hope you will enjoy and learn from the exceptional clinical case presented by Steve Smith, LMT, CMMP.
Dr. Ross Turchaninov, Editor-in-Chief
MEDICAL MASSAGE IN THE TREATMENT OF CHRONIC VISCERAL DISORDER
By Steven Smith LMT, CMMP
Littleton, CO
A fellow CMMP therapist referred a patient to my clinic whose primary complaint was the inability to swallow. She would have uncomfortable and uncontrollable belching even when swallowing her saliva.
Patient’s Medical History
On July 9, 2021, the patient started unstoppable belching with acid coming up into her esophagus, creating an excruciating burning sensation in the upper abdomen and behind the sternum.
On July 19, 2021, an endoscopy and colonoscopy didn’t find cancer but detected the presence of Helicobacter Pylori in her stomach, the only bacterium that survives and thrives in stomach acidity. When it is present in the stomach, it significantly increases the acidity of gastric juice. A second colonoscopy detected inflammation in her colon in the form of Diverticulitis.
First, she was prescribed antibiotics to kill H. Pylori. Unfortunately, her symptoms worsened even after H. Pylori was cleared.
On October 4, during emergency surgery, part of her intestine was removed, and she spent three weeks in the hospital with more antibiotics. In combination with intestinal surgery, this therapy still didn’t solve her swallowing problem. Dysphagia became so much worse that on March 10, 2022, a feeding tube was inserted into her small intestine since she couldn’t derive any nutrition via the esophagus and stomach. She injects a nutrition mix into the tube directly into the intestine for four months.
The patient was also diagnosed with a Hiatal Hernia of 13mm. Speculating that the hiatal hernia triggered Dysphagia and gastrointestinal dysfunction, her surgeon wanted another surgery to address it.
The patient refused another surgery, preferring to find a non-surgical solution. At this point, her stomach had completely shut down, causing increased frustration and stress. She told me that getting nutrition from a feeding tube was difficult and insufficient, leaving her constantly weak, exhausted, and hungry. At this point, the patient contacted Teresa Brumble, another CMMP from SOMI’s Medical Massage Certification program, who guided her to my clinic.
When the patent called the first time and described her symptoms, she asked if I could help. I told her frankly that I had never worked on anyone with similar symptoms, especially with a feeding tube inserted, but I would do some research and get back to her.
First, I consulted the Medical Massage textbook Volume I and II and found a Medical Massage protocol that looked very promising. I also read JMS’S article on a similar subject and watched videos. Later I called and set up the first appointment, explaining what I would do, and she was very encouraged.
Evaluation
Our first appointment was on July 18, 2022, with much of the time spent on her evaluation.
Local Evaluation: No tension in suprahyoid and infrahyoid muscles on the anterior neck. Gentle palpation of the epigastric area revealed very tight abdominal muscles. The patient’s stomach felt most tight just under the abdominal wall and below the edge of the rib cage. Evidently, the patient’s stomach was in severe spasm and pushed up under the diaphragm. The entire upper abdomen was very sensitive to touch.
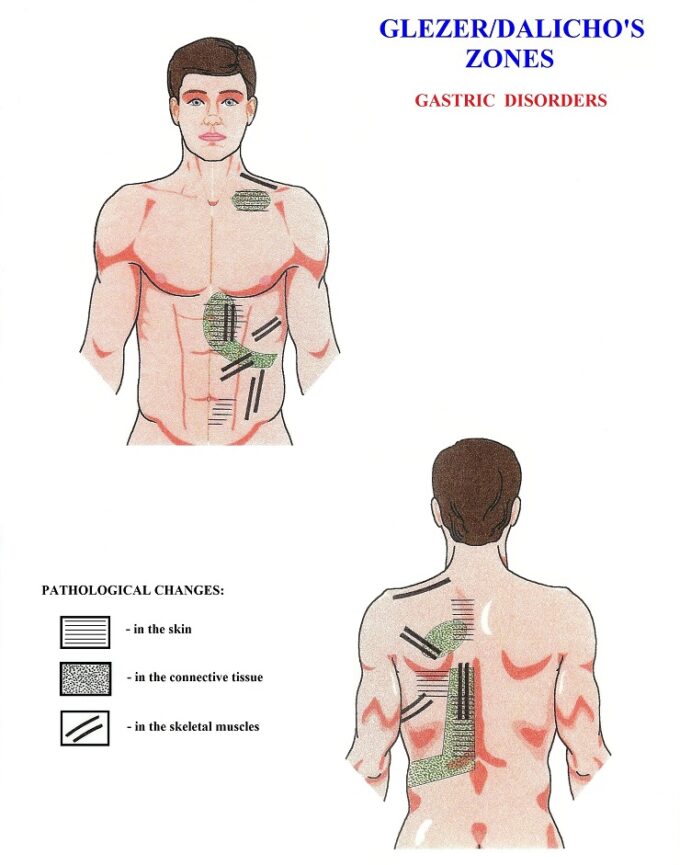
Evaluation of Reflex Zones: I used Glezer/Dalicho’s chart for gastric disorders as a guide to examine reflex reactions formed in the soft tissues due to chronic gastric inflammation. Fig. 1 illustrates Glezer/Dalicho Zones for gastric disorders.
As the Medical Massage Volume II textbook promised, all reflex zones in the skin, fascia, and skeletal muscles from Glezer/Dalicho chart presented above were active in my patient. Periosteal dysfunctions were registered in the sternum and on the left lateral surface of spinous processes of the middle thoracic vertebrae.
Based on SOMI’s training and especially on the clinical data from the article published in the JMS issue, my ideas were as follows. The patient exhibited chronic inflammation of the upper GI tract due to a severe H. Pylori infection, which significantly increased acidity in her stomach. The hiatal hernia weakened the sphincter that separates the stomach and esophagus, creating an extreme acid reflex. Although H. Pylori was successfully cleared, the patient’s symptoms continued to worsen while full-blown reflex reactions developed in the soft tissues, according to Glezer/Dalicho Zones.
Considering all these events, my theory was that the patient developed a serious and painful spasm in the esophagus and stomach, which was most likely the cause of her Dysphagia. The hiatal hernia significantly contributed to her stomach spasms.
I composed the following Medical Massage protocol to address her issue, combining local and reflex mechanisms of Medical Massage:
1. Therapeutic massage (TM) to the cervical area and both shoulders in the inhibitory regimen, consisting of effleurage and kneading to balance the activity of the parasympathetic nervous system.
2. Next, stimulation of the paravertebral areas of the left side of T5-T9, using stimulating techniques such as friction, interruptive vibration, and percussion, including areas where the cutaneous branches of the spinal nerves emerge under the skin.
3. Abdominal massage (AM) as described in Medical Massage Vol. II and the article in JMS I mentioned above.
4. Addressing the Glezer/Dalicho zones in chronic gastro-duodenal disorders, as shown in Fig.1 (Medical Massage Vol. II, R. Turchaninov, MD). I concentrated on those active reflex zones with skin rolling, connective tissue massage (CTM), and TPT for the trapezius, rhomboids major, longissimus and iliocostalis. I also added Trigger Point Therapy to both upper quadratus lumborum muscles to help control the frequent and painful belching (Medical Massage Vol. II).
I scheduled each session for 30 minutes. The first two sessions were limited to therapeutic work in the cervical and sacroiliac areas in the inhibitory regime and stimulation of the paravertebral T5-T9 regions on the left side. Each session finished with AM. During the remaining sessions, I planned to address the active Glezer/Dalicho zones, including periosteal trigger points.
First Session: I decided to start with AM to focus on the stomach and use only the local mechanism of Medical Massage.
Second Session: The following day. Patient reported that she could sleep, which she had not been able to do for some time. She felt she had more productive burps that released inner pressure in the epigastrium. I added massage in the inhibitive regime to the cervical and sacral/iliac areas this time and then friction along T5-T9 dermatomes, followed by AM.
Third Session: The following day. Patient reported having worse acid reflux all day, yet she’d still had a good night’s sleep, so she was becoming very encouraged. I used the same protocol as the previous day.
Fourth Session: Five days later. Patient reported still having painful burps with acid, yet was continuing to sleep better. I performed the same protocol but fully engaged soft tissues layer by layer, according to the Glezer/Dalicho reflex zones.
Fifth Session: Two days later. Patient reported having had a small cup of soup and being able to keep it down, the first food she could tolerate since her feeding tube was put in more than four months ago! This was critical as she felt her situation was changing, and her stomach was starting to work again, despite uncomfortable burps. I did the same protocol as the previous session and added treatment of quadratus lumborum (QL) muscles on both sides to reduce the belching.
Sixth Session: The following day. Patient reported generally feeling better for the first time in months. She was able to eat and keep down refried beans and yogurt. I used the previous session’s protocol:
AM+Inhibitory regime+Glezer/Dalicho Zones+both QL Muscles.
Seventh Session: Three days later. Patient is slowly adding more food each day. She noticed a new painful sensation in her neck and middle back that she didn’t have before. Belching was still present but not as severe and becoming less consistent. I continued with the same protocol.
Eighth Session: Two days later. Patient slowly increases food consumption and able to keep it down. Her symptoms continue to improve, especially with regard to the intensity and frequency of belching. I used the same protocol but gave more attention to the Glezer/Dalicho zones.
Ninth and final Tenth Sessions: Nine days later. The patient is doing better, and continuing to add food, although some mild belching was still present. Evaluation of the soft tissues within Glezer/Dalicho Zones indicated restoration of normal flexibility, elasticity, and function in each layer. The anterior abdominal wall became soft, and the upper abdomen had no firm spastic stomach.
The tenth session was our final session due to the patient coming down with COVID. Also, I referred her to a nutritionist to help her up-regulate her food intake more efficiently.
I contacted the patient after she recovered from COVID, and she continued improving. Finally, the feeding tube was removed by her gastroenterologist on September 6, 2022, three weeks after our last appointment. Since then, the patient has almost fully recovered with normal food ingestion and digestion. I had several follow-up appointments with her to keep everything under control.
P.S. What you just read is Medical Massage in all its glory! Steve’s clinical success was based on a combination of detailed evaluation, the implication of local and reflex mechanisms, and the simplicity and effectiveness of Medical Massage techniques.
I want readers to pause for a second before reading the following sentence. There is no other modality that could pull this patient out of her miserable life except Medical Massage, which Steve perfectly used!
Placing the feeding tube directly into the patient’s intestine meant all available treatments failed. The patient would have faced a difficult life for the rest of her days by injecting nutritional mix via a feeding tube to support essential body functions! How many patients like her are there around the country? Unfortunately, they are not privileged to be treated by correctly trained Medical Massage Practitioners.
A case like this one and other clinical submissions to JMS by our former and current students prove how important and irreplaceable SOMI’s Medical Massage Certification is for PATIENTS!
Dr. Ross Turchaninov
About the Author
Steve is a Licensed massage therapist in the State of Colorado. He has always had a passion for helping people achieve health in order to lead active lives. He was the owner of a CrossFit gym for 10 years. During this time he found massage therapy to be an important part of health and wellness. He sought to identify the source and appropriate treatments of common pain and muscle dysfunction commonly seen in the gym. He found the answer with Dr. Ross and the Science of Massage Institute. Dr. Ross has compiled extensive materials to appropriately treat many sources of pain and dysfunction through non-invasive methods. Throughout Steve’s private massage practice he has treated patients of various ages and conditions including chronic pain and movement dysfunction. You can find out more about Steve’s practice at www.virtusmm.com, or call 303-709-4930 for an appointment.
Category: Medical Massage
Tags: 2023 Issue #1