By Dr. Ross Turchaninov,
Phoenix, AZ
We continue our discussion about the important role Hyaluronic Acid (HA) plays in human health and in therapists’ work, using an exceptional article on this subject, “Hyaluronan and the Fascial Frontier” by Rebecca L. Pratt (2021), as a framework for our conversation.
In Part I, we defined HA’s role in healthy and pathological conditions: Medical Massage Courses & Certification | Science of Massage Institute » WHY THERAPISTS NEED TO KNOW ABOUT HYALURONIC ACID – PART I
Let’s examine the latter issue more closely. As discussed, HA is a major lubricant used by soft tissues to decrease heat generation during repetitive contractions. However, HA also has another very important feature—its ability to decompress soft tissues.
Why is HA so abundant in the synovial fluid of the joint? Because besides being a cartilage lubricant, HA is also the first force that resists the combined impact of body weight and gravity on the joints when we engage in physical activity and exercise. Thus HA assists in maintaining the vitality of the cartilage inside the joint, acting as an initial shock absorber (Tamer, 2013).
Interestingly enough, HA plays precisely the same role in the normal function of soft tissues. Besides acting as a lubricant to diminish friction during soft tissue sliding, HA creates and maintains extra space between the soft tissue layers. This brings us to the issue of deep fascia since it relies more than superficial fascia upon the abundant distribution of HA for its normal functionality.
DEEP FASCIA
There is a huge difference between superficial and deep fascia despite their similarity as connective tissue structures. Superficial fascia has a very large concentration of water in colloid form, and it builds a microscopic web of collagen, reticular tissue, elastin fibers, vessels, nerves, and various receptors. It is also highly deformable (Bordoni and Zanier, 2015).
The deep fascia is much thicker, denser, and less extendable than the superficial fascia. It is essential for translating muscle contractions into joint movements (Pawlina, 2018). Thus, deep fascia needs higher levels of HA than superficial fascia to do its job.
HA in the deep fascia is produced by fasciocytes located within the fascial layers. Besides saturating the entire deep fascia and making it thicker, HA and attracted water spread along the inner and outer surfaces of deep fascia, lubricating them and tissues fascia separates.
A normal concentration of HA within the deep fascia additionally reinforces its density, thickness, and shock-absorbing abilities, creating perfect conditions for productive and free muscle contractions. Therefore, in the early stages of deep fascial tension, the absence of proper lubrication greatly diminishes the weakening and thinning of the deep fascia.
One unfortunate outcome of increased fascial tension and fascia thinning is a delay in the local venous and lymph drainage from the deep fascia and muscles that HA covers (Roman et al., 2013). In such cases, interstitial fluid accumulates and is retained between myofibrils, triggering interstitial edema, which becomes a critical factor in forming future hypertonus and active trigger points. Also, local edema puts pressure on the fasciocytes, which are HA-generating stations, and contributes to fascia drying and the formation of adhesions between fascia and surrounding tissues.
If one looks at the pattern of the interstitial edema in the affected fascia, most of it will accumulate along the fascial edges (Roman 2013). This is an essential clinical guide to therapists because science guides us to the fascial edges that must be targeted first.
Another aspect we discussed in the previous article is the nature of HA. Long-chained HA is a healthy and productive substance, while short-chained HA exhibits a self-sticky nature (Dintenfass, 1963). Thus, the disappearance of long-chained HA and its replacement by short-chained HA are additional factors in shortening fascia and forming adhesions between soft tissue layers. HA depletion greatly affects the entire contraction/relaxation cycle of the deep and eventually superficial skeletal muscles, so they become negatively affected (Stecco, 2011).
Why does tension in the deep fascia covering deep skeletal muscles negatively affect the function of superficial skeletal muscles and become responsible for TPs formation there?
Let’s look closely at Figure 1, which shows the anatomy of the posterior shoulder. Skin and subcutaneous fat are cut out so readers see the superficial fascia (red arrow), which covers the posterior portion of the deltoid (#7). The deep fascia (blue arrow) separates the deltoid muscle (#7) from the underlying infraspinatus muscle (#8).
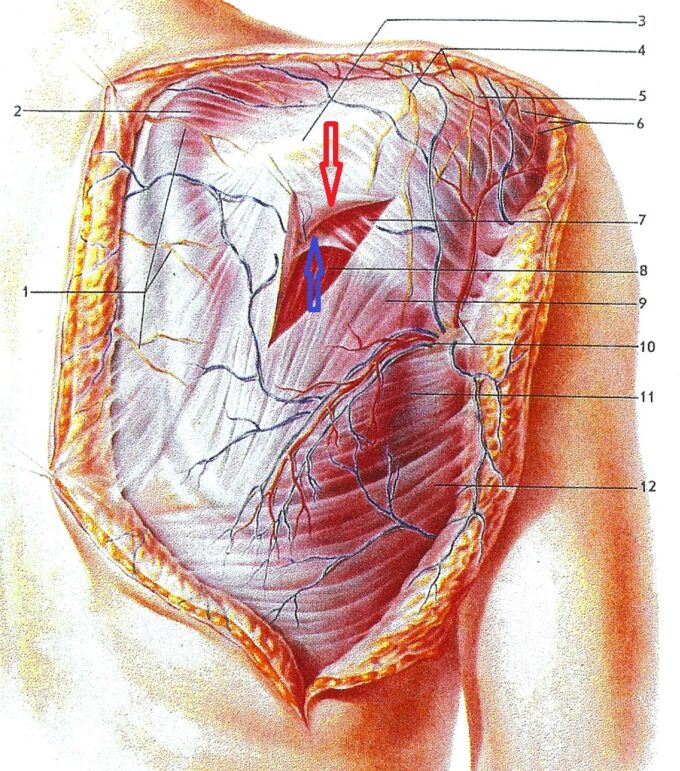
Fig. 1. Soft Tissue Arrangement in the posterior shoulder
The posterior portion of the deltoid muscle, as a more superficial layer, has two points of attachment to the periosteum of bones: the spine of the scapula and the deltoid tuberosity of the humerus. Thus, the belly of the deltoid muscle is not attached to any bone structure since it is positioned above the infraspinatus, and deep fascia separates them. Conversely, the entire belly of the infraspinatus muscle is firmly gripping the periosteum of the scapula. This arrangement of soft tissues in the posterior shoulder means that in a normal scenario, the deltoid has a much larger contraction and relaxation cycle than the infraspinatus. This is why the deltoid is the executor of movement, while the infraspinatus is mostly the stabilizer of movement.
As we just mentioned, the deltoid has a larger range of contraction. However, if the deep fascia, which separates both muscles, becomes shorter, the deltoid muscle becomes glued to the infraspinatus. Then, instead of sliding against each other, the deltoid slides with the infraspinatus. Since the infraspinatus muscle normally has a shorter range of contractions, these pathological adhesions between both muscles greatly affect the contraction pattern of the deltoid muscle, which becomes one reason for ROM restrictions in the shoulder joint.
I want readers to pause for a second and digest the information just discussed. Modern scientific data indicates that fascial tension is the trigger for Myofascial Pain Syndrome (MPS), and it is directly associated with a decrease in the concentration of the normal long-chained structure of HA and a decrease in muscle contractile ability (Stecco et al., 2013).
Thus, all muscle dysfunctions are the consequence of fascial tension, so treating somatic disorders as pure muscle abnormalities is a dead end if the therapist targets the muscles only, using various techniques and modalities (Trigger Point Therapy, Muscle Energy Techniques, Neuromuscular Therapy, etc.) becomes a dead end. Decompressing superficial and deep fascia is the critical initial step of successful somatic therapy. Working on the muscles only brings temporary relief, allowing trigger points to go to a latent or sleeping state and later be reactivated, eventually forming irreversible degenerative changes in the muscles in the form of myogelosis.
This fascinating data should completely change our approach to treating hypertonic muscular abnormalities by prioritizing decompression of the superficial and especially deep fascia. All current techniques and modalities that do not include local decompression of fascia become an endless chase of the tail. Thus, if we are not following the correct sequence of somatic rehabilitation, we sacrifice the patient’s health for the interest of our professional egos.
HOW TO REPLENISH HA AND RE-LUBRICATE FASCIA
Any technique or modality that doesn’t include detailed work on the superficial and deep fascia brings only a partial solution. It cannot deliver stable clinical results, especially in complex, chronic dysfunctions. Thus, comprehensive somatic rehabilitation based on science must include this vital treatment component.
There are two equally important aspects in the restoration of affected fascia by Medical Massage:
- Decompression of the fascia by application of the Lateral Shift Techniques between layers of the soft tissues
- Re-lubrication of the fascia
Pressure between the soft tissue layers must be decreased to replenish HA in the fascia. This can be done with initial drainage and medical massage techniques in lateral shift mode. The lateral shift means that therapists work with soft tissues in a direction perpendicular to the main orientation of the muscle contractile forces and pressure line distributions. The lateral shift techniques that displace the soft tissues are also called Fascia Unwinding (Tozzi, 2012). Superficial and Deep Fascia are decompressed by using different techniques.
Decompression of Superficial Fascia
Skin rolling, connective tissue massage (CTM), or mobile cupping with lifting component care clinical tools to decompress the superficial fascia. The impact of these therapies on the degree of tension in the collagen fibers of the superficial fascia is well-documented (Pohl, 2010).
- German Connective Tissue Massage
Strokes are conducted by the hook formed by the third and fourth fingers (the other hand placed on top can be used to reinforce the hook), pulling in the practitioner’s direction. If adhesions are significant, the angle of the hook should be decreased.
2. Skin Rolling
Skin Rolling can’t be used on patients with severe fascial adhesions due to the formation of Connective Tissue Zones or in patients with significant accumulation of subcutaneous tissues.
3. Mobile Cupping with lifting component.
Vacuum must be minimal just to lift skin with subcutaneous tissues. With plenty of lubricant, move the jar to decompress the superficial fascia while lifting it.
Decompression of Deep Fascia
Scrolling kneading is an example of a massage technique that uses lateral shifts to address deep fascia. The video below shows the technique applied to the posterior arm. Notice the full continuous control of the muscle mass during the execution of the technique.
Lateral shift forward displaces the triceps laterally while kneading it, and at the same time, it stretches the deep fascia, which separates triceps brachii from the brachialis muscle and humerus; the vertical lift and mobilization of the triceps brachii back to the practitioner additionally decompresses deep fascia; gentle compression and roll of the tissues forward knead entire triceps against humerus while additionally decompresses deep fascia. The elevation of the tissues during scrolling kneading creates extra space between the layers of the soft tissues in the posterior arm.
Myofascial Release is another helpful tool, but since the technique has limited use of the Lateral shift, it must be combined with one of the treatment options mentioned above for optimal results.
In Part III of this article, we will discuss how Medical Massage helps to re-lubricate the fascia and what nutritional support the patients may use to help with HA production.
REFERENCES
1. Bordoni B., Zanier E. Understanding Fibroblasts in Order to Comprehend the Osteopathic Treatment of the Fascia. Evid Based Complement Alternat Med. 2015: 860934.
2. Dintenfass, L. Lubrication in Synovial Joints. Nature 1963, 197, 496–497
3. Pawlina, W. Histology: A Text and Atlas: With Correlated Cell and Molecular Biology, 8th ed.; LWW: Philadelphia, PA, USA, 2018
4. Pohl H. Changes in the structure of collagen distribution in the skin caused by a manual technique. J. Bodyw Mov Ther. Jan 2010; 14: 27-34M
5. Pratt R.L. Hyaluronan and the Fascial Frontier. Int. J. Mol. Sci. 2021, 22, 6845.
6. Roman, M.; Chaudhry, H.; Bukiet, B.; Stecco, A.; Findley, T.W. Mathematical Analysis of the Flow of Hyaluronic Acid Around Fascia during Manual Therapy Motions. J. Am. Osteopath. Assoc. 2013, 113, 600–610.
7. Stecco A., Gesi M., Stecco C., Stern R. Fascial Components of the Myofascial Pain Syndrome. Myofascial Pain, Vol 17 (352), 2013
8. Tamer, T.M. Hyaluronan and Synovial Joint: Function, Distribution and Healing. Interdiscip. Toxicol. 2013, 6, 111–125.
9. Tozzi, P. Selected fascial aspects of osteopathic practice. J Bodyw Mov Ther 2012 Oct;16(4): 503-19
ABOUT THE AUTHOR
Dr. Turchaninov graduated with honors from the Odessa Medical School in Ukraine in 1982. He was admitted to the residency program of the Kiev Scientific Institute of Orthopedy and Rehabilitation, which he completed in 1985. In 1989, Dr. Turchaninov obtained his PhD degree in Medicine,
From 1986 to 1988, he worked as a supervisor of the rehabilitation program for the Ukrainian Ministry of Public Health. During these years, he also worked with the medical team of the relief effort following the Chornobyl nuclear plant disaster.
In 1992, Dr. Turchaninov was invited to work in rehabilitation centers in New York City and Scottsdale, Arizona, as head of their medical massage program.
Dr. Turchaninov founded the Science of Massage Institute, which is dedicated to bringing clinical science into massage therapy and educating therapists on the clinical applications of medical massage. He is the Editor in Chief of the Journal of Massage Science. He lectures in the U.S. and abroad on manual therapy and medical massage issues and is regularly invited to speak at American and international conferences.
Dr. Turchaninov is the author of more than 100 scientific papers and publications in European and American medical journals. He is the author of three major textbooks: Medical Massage, Volumes I and II, and Therapeutic Massage: A Scientific Approach.
Dr. Turchaninov lives in Phoenix, Arizona. His interests are literature, art, history, and travel.
Category: Medical Massage
Tags: 2024 Issue #1


