by Dr. Ross Turchaninov
Phoenix, AZ
Dear readers, if you are practicing the clinical aspects of massage therapy, we invite you to carefully analyze the information in this and the following articles. It carries great value for any health professional engaged in somatic rehabilitation.
Let us consider a patient with lower back pain as an example. Two fundamental questions arise:
- The patient experiences severe lower back pain. Where is the pain actually located?
- The same patient presents with lateral trunk tilt. Why does this occur?
From article to article, from class to class, and from treatment room to treatment room, many educators and therapists treat local symptoms—such as lower back pain, lateral tilt, or shoulder elevation—as the primary therapeutic targets. However, this is narrow clinical thinking that reduces the effectiveness of treatment, especially in chronic pain and dysfunction, where multiple secondary abnormalities develop over time.
If proper therapy is not provided, these secondary symptoms eventually dominate the clinical picture. They can mislead therapists into treating the consequences while the original trigger remains hidden under layers of the brain’s compensatory reactions.
The discussion in this article is based on two fundamental scientific models of pain formation:
- Gate-Control Theory of Pain (Melzack and Wall, 1965)
- Neuromatrix Theory of Pain (Melzack and Katz, 2013)
Before continuing, we recommend reviewing SOMI’s earlier publications on these models from a massage therapy perspective.
Gate-control Theory of Pain: Medical Massage Courses & Certification | Science of Massage Institute » HOW MASSAGE HEALS THE BODY: CLINICAL APPLICATION OF GATE CONTROL AND NEUROMATRIX THEORIES OF PAIN
Neuromatrix Theory of Pain: Medical Massage Courses & Certification | Science of Massage Institute » HOW MASSAGE HEALS BODY. PART IV PHENOMENON OF PAIN AND MASSAGE THERAPY: NEUROMATRIX THEORY
PHENOMENON OF PAIN
Pain is a highly complex physiological, psychological, and even philosophical phenomenon. For humans, it is both a curse and a blessing. While it devastates us physically and emotionally, it also saves lives by preventing dangerous actions.
The human body processes pain through two distinct systems, and each has its own network of specialized receptors located in the tissues and organs:
- a fast pain-analyzing system, responsible for acute, sharp pain perception;
- a slow-pain-analyzing system, responsible for dull, low-intensity, chronic pain.
Importantly, pain does not reside in the lower back—or any other local area—by itself. Pain as sensation is created solely by the brain! Symptoms such as pain, numbness, or burning are generated centrally, based on information received from pathologically altered peripheral receptors. This is a pathophysiological fact.
Thus, dysfunction of peripheral receptors in soft tissues and internal organs is the direct trigger for pain and other pathological sensations. A well-trained therapist understands that while working on soft tissues locally (draining interstitial edema, releasing fascial adhesions, etc.), they are resetting the function of peripheral receptors and, through them, recalibrating the patient’s sensory and motor cortex. That will eventually stop the brain from further re-printing the pain pattern.
This is the foundation reflex mechanism of MM, which must be combined with local work on the affected tissues. The reflex mechanism MM provides long-term stability of clinical results. Addressing symptoms only at the local level with a single modality is like trying to fly with one wing. Thus, the ultimate goal of successful somatic rehabilitation via Medical Massage (MM) is the patient’s brain, and it is achieved by the therapist’s ten magic fingers through resetting the patient’s peripheral receptors.
LAYERS OF SOFT TISSUE AND DISTRIBUTION OF RECEPTORS
There are four primary soft tissue layers in the human body:
- Skin
- Fascia
- Skeletal muscles
- Periosteum
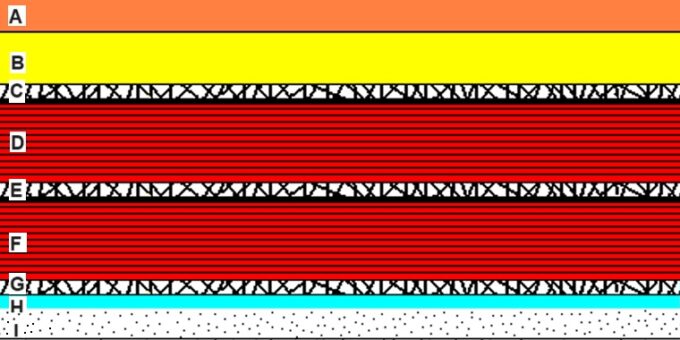
Fig. 1 illustrates the typical arrangement of the soft tissues in the human body using the posterior leg as an example.
A – Skin; B – Subcutaneous Tissue; C – Superficial Fascia with fibrotic bridges; D – Superficial muscle (gastrocnemius m.); E – Deep Fascia with fibrotic bridges; F – Deep Skeletal Muscle (soleus m.); G – line of fibrotic bridges; H – Perisoteum; I – Bone (tibia and fibula)
Each layer is unique in structure, function, innervation, circulation, and—most importantly—the distribution of peripheral receptors, including nociceptors (pain receptors). Let’s review peripheral receptors in the soft tissues, which constantly feed the brain with necessary data.
Skin
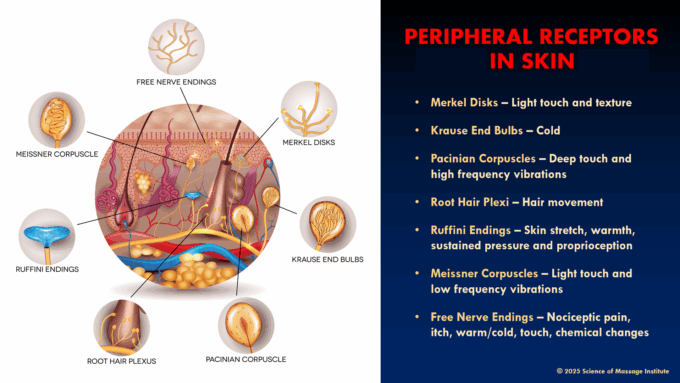
The skin contains the richest and most complex network of peripheral receptors, allowing the brain to interpret the environment and respond appropriately. Fig. 2 summarizes peripheral receptors located in the skin.
Fascia
Fascia is also richly innervated. In addition to the receptors found in skin, the fascia contains:
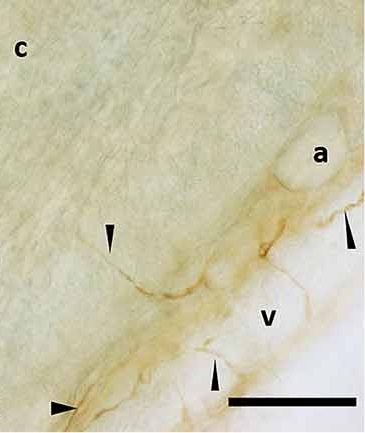
- Interstitial receptors are the ends of sensory nerves that innervate fascia. They monitor fascial tension and stretch. Interstitial receptors are predominantly located in the deep fascia, which separates muscle layers. For example, the deep fascia that separates the gastrocnemius and soleus muscles or the trapezius and rhomboid muscles. The full function of interstitial receptors is still being examined by scientists. Fig. 3 illustrates the sensory innervation of the superficial fascia.
a – adipose tissue
c – connective tissue of superficial fascia
v – vessel supplies the fascia
small arrows – sensory nerves innervating the fascia
Interstitial receptors link fascial and muscular dysfunction to the Autonomic Nervous System (ANS). Thus, their activation can trigger autonomic responses, such as blood pressure fluctuations, nausea, sweating, or rapid, shallow breathing. ANS imbalance additionally sensitizes the brain to nociceptive input, amplifying pain perception.
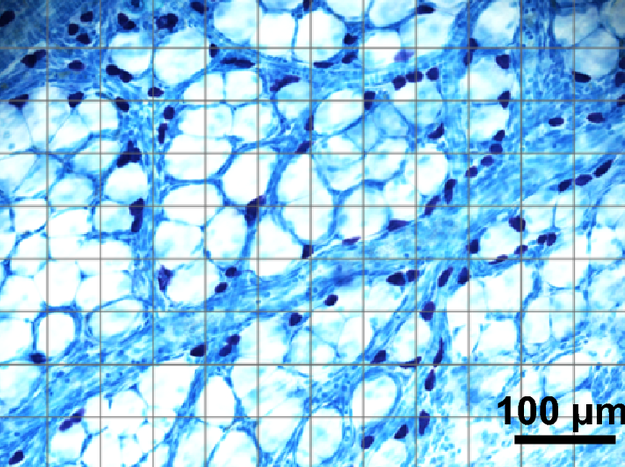
- Chemoreception. Fascia lacks the classic chemoreceptors that respond to local biochemical changes. However, fascia contains an abundant accumulation of mast cells, and their activation alters local pH, releases cytokines during local inflammation, participates in tissue repair, and forms an initial immune defense barrier. Their activation further sensitizes nociceptors and enhances pain generation. Fig. 4 illustrates the distribution of mast cells in the fascia.
Skeletal Muscles
Two key receptor groups govern muscle function:
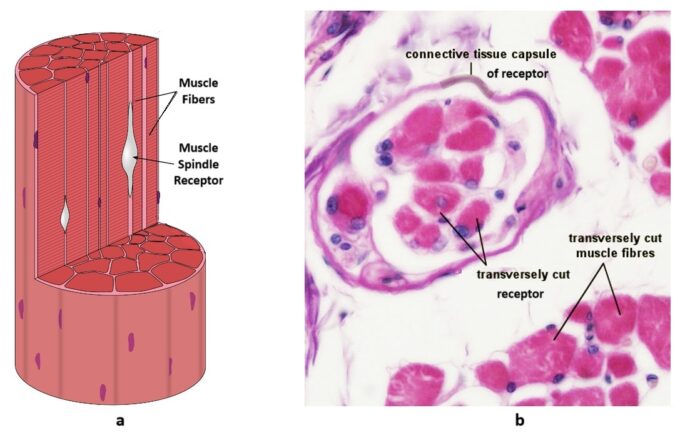
- Muscle spindle receptors, located in the muscle belly they monitor changes in muscle length and stretch. They are critical for muscle coordination and posture. In dysfunction, they start to send incorrect data to the motor cortex, confusing the brain and deepening the dysfunction. Fig. 5 illustrates the position and cross-section of skeletal muscles with the muscle spindle receptor.
a – position of muscle spindle receptors in the muscle bellies between myofibrils
b – cross-section of skeletal muscle with the muscle spindle receptors surrounded by a capsule
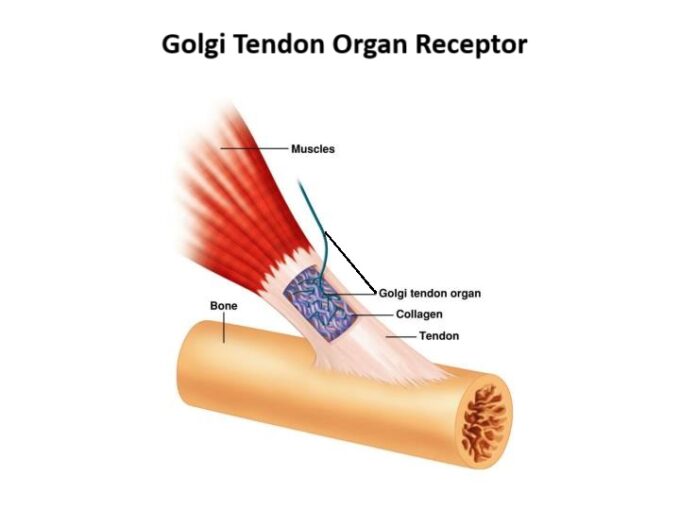
- Golgi tendon organ receptors, located at muscle–tendon junctions, detect tension and act as inhibitory receptors. We commonly engage them during passive stretching to induce relaxation. The sensory fibers of the receptor weave between the tendon’s collagen fibers. Fig. 6 illustrates the position and structure of the Golgi Tendon Organ receptor.
Fig. 6. Golgi Tendon Organ receptor in the tendinous part of the muscle
Periosteum
The periosteum has relatively few receptors overall but is densely populated with nociceptors. The intense pain a bone fracture patient feels is not due to the bone fragmentation (which lacks nociceptors) but to damage of the thin periosteum surrounding it. Periositeum also has a great number of Meissner’s Corpuscle receptors, which detect vibration.
CLINICAL IMPLICATIONS
The varied receptor distribution across each soft tissue layer underscores the need to treat each layer individually. Treating soft tissue as a single bulk structure is ineffective and ultimately a dead end in somatic rehabilitation.
Effective therapy requires that the therapist:
- accurately evaluate the tissue layers involved,
- understand receptor distribution and function in those tissues, and
- select appropriate techniques and modalities for each layer.
No single method — whether Neuromuscular Therapy, Trigger Point Therapy, or Myofascial Release — is sufficient on its own. Each has value in a specific clinical niche. Stable and lasting results come only from their thoughtful integration.
Thus, therapists must look beyond local pain and structural changes. The true therapeutic goal is the patient’s brain. By restoring the function of peripheral receptors in skin, fascia, muscles, and periosteum, we gradually reduce central pain perception.
This integrative, receptor-based approach is the foundation of Medical Massage, which is a treatment concept rather than an individual modality, as mistakenly presented. Medical Massage combines scientifically validated, clinically tested methods to address each layer of soft tissue individually and systematically, tailored to each patient’s needs.
NEXT IN Part II
In the following article, we will examine the mechanisms of acute and chronic pain, the development of structural abnormalities, and how Medical Massage addresses them effectively.
Consider joining the Science of Massage Institute for in-depth training in Medical Massage and its clinical application. Here is our remaining schedule for 2025: Medical Massage Courses & Certification | Science of Massage Institute » Medical Massage Continuing Education
REFERENCES
Fede C., Petrelli L., Winfried C., Neuhuber F., Tiengo C., Biz C., De Caro R., Schleip R., Stecco C. Innervation of human superficial fascia. Front. Neuroanat., Vol. 16, 2022
Melzack R. (1990) Phantom Limbs and The Concept of Neuromatrix. Trend Neurosci.. 13:88-92.
Melzack, R., Katz, J. (2013). Pain. Wiley Interdisciplinary Reviews: Cognitive Science, 4(1):1-15, Jan/Feb., 2013
Melzack R., Wall P.D. Pain Mechanisms: A New Theory. Science. Nov. 1965, 150(3699): 971-979
Zhang D., Dong Y., Zhang Y., Su X., Chen T., Zhang Y., Wu B., Guoheng X. Spatial distribution and correlation of adipocytes and mast cells in superficial fascia in rats. Histochemistry and Cell Biology, 2019, 152(6):1-13
ABOUT THE AUTHOR
Please click here to read Dr. Ross Turchaninov’s bio: https://www.scienceofmassage.com/editorial-board/
Category: Medical Massage
Tags: 2025 Issue #2