We continue to review how massage therapy heals the human body via various healing mechanisms we summarized in Diagram 1. We started this discussion in Jan/Feb (Part I) and Mar/Apr (Part II) 2010 issues of JMS and we covered the cellular stimulation, phenomenon piezoelectricity and streaming potentials.
This and previous articles on the theoretical explanation of mechanisms responsible for the therapeutic power of massage therapy contained a lot of medical terminology and concepts. We recognize that readers may have some difficulties in reading these articles and effectively using information they contained.
In JMS we try to present information in the most useful form and we strongly believe in the great professional potential of our readers. This is why we would like to equip you with as much scientifically updated information as possible. Also, we are sure that it is time for scientific data to replace personal opinions and anecdotal experience which we frequently see in many massage publications. To enhance the practical value of the article we included Practical Tips, which we hope will link theoretical information with its clinical application. Be sure to pay attention to these parts of the article.
Previously, in issue #3 of JMS we started to discuss scientific data which explains how massage therapy triggers local and general vasodilation. We reviewed how massage therapy affects vasodilation through its mechanical actions and the effect of ischemic compression on local circulation in the area of the trigger point.
In Diagram 1 we summarized the clinical effects of therapeutic massage. We based this schematic on publications which scientifically examined therapeutic mechanisms of massage therapy. As mentioned above we have already discussed the impact of therapeutic massage on the cellular function and electrical environment (see January/February and March/April 2010 issues of JMS). To replay the diagram please click at the beginning of the sliding bar (blue line) located just below the diagram.
Diagram 1. Local healing mechanisms of massage therapy
In this article, which concludes Part III, we are going to concentrate on what reflex mechanisms massage therapy uses to enhance local and general vasodilation. The concept of reflex mechanism means that the practitioner who uses the scientifically based application of massage techniques is able to actively involve the client’s nervous system to stimulate local and general circulation. Two major reflex mechanisms which massage therapy uses to stimulate vasodilation are axon reflex and central mechanism.
AXON REFLEX
Axon reflex is a less known factor responsible for reflex vasodilation. It was described and studied in 1941 by Dr. Leroy. This important information is rarely mentioned in massage publications, but it has great practical value. We will examine axon reflex with the help of Diagram 2 presented below.
The main job of peripheral receptors (touch, pressure, vibration, temperature, pain, muscle spindle receptors, Golgi tendon organ receptors) in the soft tissue is to report to the CNS any fluctuations in the outside environment or any changes in the local function. If the stimulation of peripheral receptors (‘A, B, C, D’ in Diag. 2) is strong enough to reach their threshold, the peripheral receptors form sensory input to the CNS ( ‘F’ in Diag. 2) which is then sent to the posterior horn of the spinal cord (‘G’ in Diag. 2). These areas of the spinal cord work as a sensory computer, and are responsible for the initial processing of arrived information to determine its nature and level of threat. After initial processing of arrived information, the posterior horns of the spinal cord send information to the brain for future evaluation, e.g., to the upper motor center and to the anterior horns of the spinal cord (‘H’ in Diag. 2) where lower motor centers are located. In both scenarios the body will form so -called motor response (‘I’ in Diag. 2) back the tissue where peripheral receptors were initially stimulated.
The motor responses are a result of the activation of the upper (in the brain) or lower (in the spinal cord) motor centers, which are quite different. In the first case (upper motor centers) the decrease in the outside temperature forces one to wear additional clothing, but he or she may think for a while what exact sweater or jacket to choose before making the final decision of actually putting on additional clothes. In the second case (lower motor centers) cutting the finger produces immediate motor responses in the form of a quick hand withdrawal to minimize further damage. The obvious difference in both responses depends on the level of possible damage.
The motor responses also control local and general vasoconstriction/vasodilation. In the first discussed example, response to the lower temperature will trigger chill and ‘goose bumps’ which will be accompanied by local, and eventually general, vasoconstriction. The same reflex vasoconstriction happened after cutting the finger and its goal is to minimize blood loss and stop bleeding.
When the practitioner places hands on the client’s body, it will initially respond with local reflex vascoconstriction. This is the normal protective reaction of CNS. If the practitioner continues to apply massage strokes to the affected area and uses the correct massage protocol, the spinal cord will recognize that the activation of sensory receptors in the affected area is harmless, and that the spinal cord will greatly diminish motor response (i.e., signal to trigger the vascoconstriction) with following local vasodilation in the massaged area.
To reinforce vasodilation in the massaged area the body also employs the axon reflex, which is an important mechanism the practitioner should use to increase and maintain local vasodilation. Dr. LeRoy (1941) was the first scientist who pointed to the possible involvement of the axon reflex in local and general vasodilation triggered by massage therapy. Peripheral vasodilation triggered by axon reflex can be the result of inflammation in the nerve itself (as a pathological condition) or by repetitive and intense mechanical stimulation of the soft tissues, e.g., massage stroke (Jacobs, 1954). Beside peripheral vasodilation the axon reflex is responsible for the increase of sweat production as a result of sweat gland stimulation (Schmidt et al, 2011).
Let’s review the mechanism of the axon reflex with the help of the interactive Diagram 2 presented below. To start the interactive diagram, please click ‘play’ button below diagram. To replay the diagram please click at the beginning of the sliding bar just below the diagram.
Diagram 2. Axon Reflex
First we will indicate the major anatomical components presented on the diagram. The solid arrow indicates massage strokes.
A – Indicates the skin with peripheral receptors.
B – Indicates subcutaneous tissue with peripheral receptors.
C – Indicates the subcutaneous fascia with peripheral receptors.
D – Indicates the superficial skeletal muscles with peripheral receptors.
E – Indicates the loop of the axon reflex.
F – Indicates the ascending sensory fibers from the peripheral receptors to the spinal cord.
G – Indicates the posterior horn of the spinal cord which processes sensory information arriving from the peripheral receptors.
H – Indicates the anterior horn of the spinal cord which controls the motor response to the tissues and organs.
I – Indicates the descending motor fibers from the spinal cord to the soft tissue.
Blue dot – Indicates sensory stimuli which travel from peripheral receptors to the spinal cord.
White dot – Indicates the nerve impulses which travel inside the spinal cord between the sensory center in the posterior horn and the motor center in the anterior horn.
Red dot – Indicates vasodilatory response from the spinal cord to the soft tissue where the peripheral receptors are stimulated.
Green dot – Indicates the pathway of the vasodilatory impulses which travel to the soft tissue using the loop of the axon reflex.
Now let us put the chain of events into motion (turn on to interactive diagram). When the sensory receptors are activated by massage strokes they send signals to the CNS (moving blue dot) using the ascending (i.e., to the spinal cord) sensory fibers of the peripheral nerve (letter ‘F’ on the diagram). After the stage of initial reflex vasoconstriction, the spinal cord starts to recognize massage strokes as harmless and decreases vasconstriction tone, triggering vasodilation. This is the time the axon reflex kicks in enforcing vasodilation
Here is how it works. Despite the fact that the spinal cord stopped accepting information from the peripheral receptors during the application of massage strokes, the peripheral receptors in the massaged tissue continue to fire information to the spinal cord. Small parts of fibers which compose the peripheral nerve split from the nerve trunk and form the so-called axon reflex arc (letter ‘E’ on the diagram). These short collated nerve branches get in touch with the arterioles and capillaries located in the tissue where the peripheral receptors were activated (by massaged strokes in our case). When stimuli (moving green dot) reach the arterioles using the axon reflex pathway, the peripheral vasodilation is additionally enforced. This vasodilation is more likely triggered by a histamine released pathway from the neighboring mast cells (Solcanyi, 1996). This additional vasodilation is triggered BEFORE vasodilation stimuli from the lower motor centers in the anterior horns of the spinal cord (moving red dot) are able to reach the arterioles in the massaged soft tissue. In this case, the reflex vasodilaion is a result of the combined impact of motor response from the lower motor centers in the spinal cord and by the axon reflex.
As several studies have shown, the practitioner may expect vasodilation only if he or she used intense massage techniques. The effleurage won’t trigger the axon reflex (Severini and Veranado, 1967). As Hansen and Christiansen (1973) found in a very elaborate study which involved examination of vasodilation using radiosotope 133Xe clearance from the skin, subcutaneous and muscle tissue effleurage triggers vasodilation only while it is applied. Vasodilation stops in 2 minutes after cessation of effleurage strokes. Vasodilation was registered much longer after the application of percussion and kneading techniques, which are more effective tools because they additionally engage the axon reflex.
Carlsson et al. (2006) considered axon reflex as one of the most important vasodilatory mechanisms which explain the clinical outcomes of acupuncture treatment.
Practical Tip 1
Beyond its theoretical importance, the information about axon reflex has great clinical value. To activate axon reflex, the practitioner should use repetitive application of intense stimulating techniques (e.g., friction) to stimulate peripheral receptors as much as possible and at the same time to increase the level of histamine which is used by the axon reflex as a mediator to trigger peripheral vasodilation. However, there is an important issue to remember. Always start to work in the new part of the body with effleurage and gradually increase speed, intensity and application to more intense affective techniques.
As we discussed above, the first reaction of the body to massage strokes in the new area is vasoconstricion. Thus the application of the more intense and elaborate techniques will prolong the vasocontriction period and as a result, the practitioner loses time. The initial effleurage helps to cease vasocontriction earlier and prepare tissue for the application of techniques which will trigger axon reflex.
CENTRAL MECHANISM OF VASODILATION (CMV)
CMV means that the central nervous system is directly responsible or partly involved in local or general vasodilation. There are three major mechanisms which massage therapy uses to stimulate vasodilation locally and generally. They are central inhibition of vasoconstriction, vaso-motor reflex and viscero-somatic reflex.
Central Inhibition of Vascocontriction (CIV)
Central inhibition of vasoconstriction assists local and general vasodilation indirectly by inhibiting activity of the sympathetic nervous system which predominantly controls our body during day hours as well as while we have any type of emotional or physical stress. Thus, vasodilation as a result of CIV is a product of decreased vasoconstriction. CIV is one of the keystones of the stress-reduction massage. Medical massage therapy also relies on this mechanism. For example, the inhibitory regime of massage therapy, which is the initial component of trigger point therapy, uses CIV to optimize the effectiveness of the treatment.
The concept of CIV as a main component of stress reduction and muscle relaxation was initially formulated in 1939 – 1940 by Dr. E Jacobson after almost 15 years of experimental and clinical observations. Later Jacobs (1960) and Valentine (1884) also concluded that inhibition of the vasomotor center by massage decreases activity of the sympathetic (stress) division of the autonomic nervous system, which, in turn, plays an important role in vasodilation and the overall decrease of stress level.
A recently published excellent book (Korthuis, 2011) which summarizes scientific data on blood circulation in the skeletal muscles also addresses this issue. It is worthwhile to cite.
“The skeletal muscle vasculature is richly innervated by the sympathetic nervous system and exhibits high sympathetic tone in resting conditions. This relatively high level of basal activity, couples with myogenic tone, maintains the arteries and arterioles supplying skeletal muscle in a partially constricted state. Thus, centrally directed withdrawal of sympathetic tone (bold by JMS) to the skeletal muscle…results in vasodilation.”
Vasomotor Reflexes (VR)
VR are under control of the vasomotor center which is in charge of the peripheral vasoconstriction and vasodilation in arterioles. Thus these reflexes are directly responsible for the blood flow though the tissue and inner organs. The vasomotor center is located in the medulla oblongata part of the brain (see Diagram 3) which also controls cardiac function as well as coughing, sneezing, vomiting and swallowing.
Diagram 3. Medulla oblongata
As we have discussed, VR are mostly controlled by the sympathetic division of the autonomic nervous (stress) system and under normal physiological conditions the arterioles throughout the body under 50% of maximal constriction (Bullock et al. 1984). Thus, when we discuss the matter of vasodilation we should refer mostly to the level of the vasoconstruction or vasomotor tone (Davis, Hill, 1999; Korthuis, 2011). In such cases the peripheral vasodilation is a direct sequence of the decreased level of the physiological vascoconstruction or activity of sympathetic (stress) nervous system. In simpler words, this means lesser vasomotor tone, stronger and longer vasodilation.
The existence of VR triggered by massage therapy was originally shown by Prof. Zabludovsky (1913) who used a plethsymograph to register the phenomenon of increased blood flow in the forearm opposite to the massaged and in both calves of the same subject. VR and their correaltion with massage therapy were extensively studied by Ebeland and Wisham (1956). Using various tests including rate of radiosodium clearance from the massaged and non-massaged tissues, the authors concluded that massage therapy triggers local and general vasodilation via VR.
Chernigovsky (1980) intensively researched the function of peripheral receptors and especially baroreceptos which control the degree of constriction/dilation of blood vessels and consequently blood flow. At first the author used massage as one of the tools to study the activity of peripheral receptors and their adaptation. However, initial data convinced the author to examine massage therapy as a tool to help evaluate and explain the outcomes of the study.
Based on obtained data, Dr. Chernigovsky developed a very interesting theory which tried to explain what profound impact massage strokes have on general and local vasodilation. According to this theory, the body’s capillary network serves as a major reflex zone of the entire cardio-vascular system. The upper vosomotor centers, heart and all vascular components all the way to arterioles adjust their function according to the changes in the capillary network. In this case, correctly applied massage strokes trigger local vasodilation, but the entire capillary network reacts with reflex vasodilation and it helps to decrease peripheral vascular resistance to cardiac work.
Severini and Venerado (1967) showed that application of massage techniques on the one leg triggers the vasodilation in the opposite leg. Recently Prilutsky (2003) conducted a pilot study for Beverly Laboratory of the Vascular Studies in Los Angeles. The author examined the effect of Swedish massage in the form of application of various effleurage techniques and medical massage techniques on the arterial blood circulation in the lower extremities of healthy adults. Pulse Volume Recording (PVR) Photopletismograph and Termography were used to compare arterial blood circulation in both groups, The largest changes were registered in PVR. What is important about this study is that all measurements were conducted in the lower extremity opposite to the massaged one. Let’s review the data from one of the subjects.
The study involved two massage practitioners, one who practices Swedish massage and one who practices medical massage. The original value of PVR in the lower right extremity of the subject was 0.81. After Swedish massage was performed for 15 minutes on the lower left extremity the PVR dropped to 0.73, i.e., arterial blood perfusion even slightly decreased on the opposite, non-massaged lower extremity. At this moment the medical massage practitioner started to work on the same subject for 15 minutes and the PVR almost immediately started to climb. At the end of 15 minutes PVR on the lower extremity was 1.22. Thus arterial blood perfusion was almost double if compared to 0.73 value when the medical massage practitioner took over. After the treatment PVR continued to climb, and at the end of the second hour it was 1.63.
In the recently conducted study, the impact of connective tissue massage on blood circulation in type 2 diabetic patients was examined by Castro-Sanchez et al., (2011). Ninety-eight type 2 diabetes patients with stage I or II peripheral arterial disease were randomly assigned to a clinical and control group. Using various tests and equipment the authors compared blood circulation in the toes of patients with type 2 diabetes.
Interestingly, the authors tested the effectiveness of connective tissue massage (clinical group) against magnetotherapy (control group) while patients in both groups continued to receive standard medical care for type 2 diabetes. The statistical evaluation of obtained data allowed the authors to conclude that:
“Connective tissue improves blood circulation in the lower limbs of type 2 diabetic patients at stage 1 or 11-a (P<.05) and may be used to slow the progression of peripheral arterial disease.”
Practical Tip 2
If the practitioner would like to trigger long lasting vasodilation as a result of therapeutic or stress reduction sessions he or she should use various kneading and percussion techniques. The kneading techniques should be applied separately on the level of skin and level of superficial and deep skeletal muscles. The effleurage techniques many practitioners rely on in their massage routine are incapable of producing effective and what is more important, long lasting vasodilation. These techniques must be used during the massage session, but the practitioner should limit their application. Otherwise, his or her efforts are wasted.
Practical Tip 3
If the practitioner deals with patients who have impaired circulation (e.g., as a result of diabetes, thrombosis obliterans, etc.) he or she should use more sophisticated and effective massage methods to improve blood circulation (e.g. Connective Tissue Massage, Segment-Reflex Massage, Neuromuscular Therapy). In such cases the practitioner uses methods of medical massage therapy which are specifically designed to deal with such conditions. In these cases the practitioner combines local vasodilation with its reflex enforcement to restore or improve blood supply to the affected areas.
Practical Tip 4
Glezer/Dalicho zones for patients with circulatory abnormalities (they are discussed below) are a great guide to design effective massage protocol.
Practical Tip 5
To enhance the vasodilatory effect of medical massage the practitioner should always start treatment on the opposite, unaffected part of the body which matches the exact location of the affected area. In such cases the practitioner uses reflex vasodilation first, as a preparation to work in the affected area to improve blood circulation.
Viscero-Somatic Reflexes (VSR)
Another way massage therapy enhances vasodilation is via VSR. These reflexes are the foundation for the application of medical massage in cases of inner organ disorders. These reflexes link somatic structure (skin, fascia, skeletal muscle, and periosteum) with corresponding inner organs. VSR are possible because somatic structure and inner organs share innervation provided by the same segment of the spinal cord. For example, the same segments of the spinal cord are responsible for the innervation of the lungs, skin and fascia in the middle back, trapezius muscle and periosteum of the scapula. Thus, health practitioners may expect that the patients with chronic pulmonary abnormalities (e.g., emphysema) will exhibit pathological changes in the form of reflex zones in these areas of the body. Function and existence of reflex zones in the soft tissue are driving forces which contribute to the further progress of pulmonary abnormalities.
English physician Dr. H. Head formulated the concept of VSR and in 1893 he published maps of possible abnormalities in the skin in the case of various visceral disorders. These maps, which are called Head’s zones, are classic examples of VSR. Other maps were later published (e.g., Dicke’s maps) but the most comprehensive work was done by two German physicians who, in 1953, published what they called Glezer/Dalicho’s zones.
Diagram 4 presented below shows Glazer/Dalicho zones in cases of chronic pulmonary disorders. It indicates the most common locations of pathological abnormalities in the form of reflex zones in the soft tissue of patients with chronic pulmonary disorders. Dr. Glezer and Dalicho published diagrams for every system of the human body as well as the most common location of somatic abnormalities.
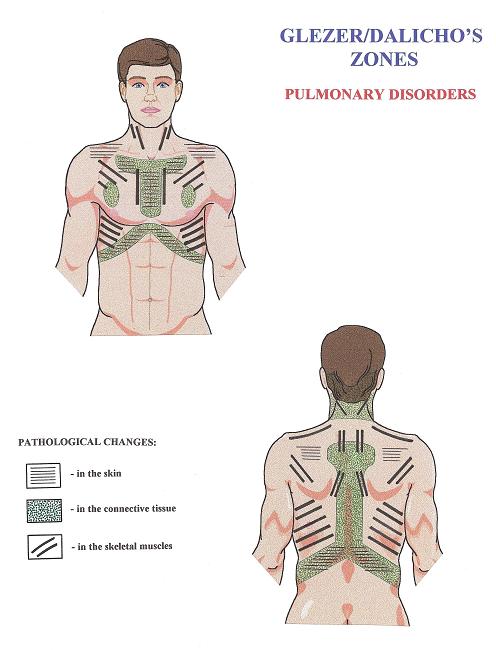
Diagram 4. Glezer/Dalicho zones in cases of chronic pulmonary disorders.
Each set of diagrams shows the location of reflex zones in the skin (parallel thin lines), in the connective tissue (dotted areas) and in the skeletal muscles (parallel thick lines). The existence and participation of VSR in the control of inner organ function as well as VSR’s importance as therapeutic pathways on normalization of the affected inner organs are reported by numerous studies (Korr, 1947; Ebner, 1956; Beal, 1985; Johnston and Golden, 2001; Giamberardino, 2003; Giamberardino et al, 2005; Jarell, 2009; Desmaris et al, 2011).
The practitioner who uses correctly formulated MEDICAL MASSAGE PROTOCOL is able to eliminate pathologically developed reflexes in the soft tissue and, at the same time, normalize function of the affected inner organ by restoring its normal innervation and triggering long lasting vasodilation which helps to mobilize the reparative abilities of the tissue of the affected organ.
Practical Tip 6
If the practitioner would like to optimize therapy and keep the client’s interests as a priority, the applied massage treatment must be formulated and adjusted individually. It is a professional mistake to apply massage on all clients without personal modifications according to the client’s health needs. Otherwise the massage session becomes senseless rubbing.
Let’s say that the massage practitioner works in the spa and a new client is scheduled. Usually the therapist asks every new client about chronic somatic abnormalities as well as chronic visceral disorders. Equipped with such basic data, the practitioner must take into consideration the location of reflex zones associated with the chronic visceral abnormality the client suffers. In such cases the practitioner adjusts the therapeutic massage routine according to the location of reflex zones in the soft tissue. The therapist may use Head’s Zones, Dickie’s Map or Glezer/Dalicho zones as clinical guides.
By concentrating on the areas of reflex zones and emphasizing their importance to the client, the practitioner prevents reflex zone formation or decreases their intensity. Even the simple fact of spending more time in these areas makes a big difference to the patient’s health.
If the therapist practices medical massage, the diagnosis of visceral abnormalities allows him or her to participate in the treatment of the disease using medical protocols. Having witnessed the results of medical massage therapy for patients with chronic visceral disorders, the author believes that clinically effective application of MEDICAL MASSAGE PROTOCOLs in cases of chronic visceral disorders is the highest level of the massage therapist’s expertise. Of course, this is the author’s personal opinion.
Beal M.C. Viscerosomatic reflexes: a review. JAOA, 85(12):53-58, 1985
Bullock J., Boyle J., Wang, M.B., Ajello, R.R. Physiology. ‘John Wiley Sons’, Pennsylvania, 1984
Carlsson CP, Sundler F, Wallengren J. Cutaneous innervation before and after one treatment period of acupuncture. Br. J. Dermatol, 155: 970-976, 2006
Castro-Sanchez A.M., Moreno-Lorenzo C., Mataran-Penarrocha G.A., Feriche-Fernandez-Castanys B., Granados-Gamez G., Quesada-Rubio J.M.Connective tissue reflex massage for type 2 diabetic patients with peripheral arterial disease: randomized controlled trial. Evid Based Complement Alternat Med., 2011: 804321, 2011
Chervigovsky V.N. Interoreceptors. ‘Medicina’, Moscow, 1980
Davis M.J., Hill M.A. Signaling mechanisms underlying the vascular myogenic response. Physiol Rev., 79: pp. 387-423, 1999
Desmaris A., Descarreaux M., Houle S. Piche M. Tuning the gain of somato-sympathetic reflexes by stimulation of the thoracic spine in humans. Neurosci Lett., Feb 25;490(2):107-11, 2011
Ebel A., Wisham L.H. Effect of massage on muscle temperature and radiosodium clearance. Arch. Phys. Med., July: 339-405, 1952
Ebner M. Peripheral vasculatory disturbances: treatment by massage connective tissue in reflex zones. Br. J. Phys. Med., 19(18):176-180, 1956
Gelzer O. Dalicho V.A. Segmentmassage. Leipzig, 1955
Giamberardino M.A. Referred muscle pain/hyperalgesia and central sensitisation.J Rehab. Med., May;(41 Suppl):85-8, 2003
Giamberardino M.A., Affaitatti G., Lezra R., Lapenna D., Costantini R., Vecchiet, L. Relationship between pain symptoms and referred sensory and trophic changes in patients with gallbladder pathology. Pain, Mar;114(1-2):239-49, 2005
Hansen T.I., Kristiansen J.H. Effect of massage, short wave diathermy and ultrasound upon 133Xe disapperance rate from muscle and subcuteneous tissue in the human calf. Scand J Rehab Med., 5:179-182, 1973
Head H. On disturbances of sensations with special reference to the pain of visceral disease. Brain, 16:1-133, 1893
Jacobs M. Massage for the relief of pain: anatomical and physiological considerations. Phys.Ther. Rev., 40: 93-98, 1960
Jacobson E. Variation of Blood Pressure With Skeletal Muscle Tension and Relaxation. Ann. Interal Med., 12:1194-1212, 1939
Jacobson E. Variation of Blood Pressure With Skeletal Muscle Tension and Relaxation. Ann. Interal Med., 13:16-19-1625, 1940
Jarrell J. Demonstration of cutaneous allodynia in association with chronic pelvic pain. J. Vis. Exp., Jun 23;(28), 2009
Johnston W.L., Golden W.J. Segmental definition–Part IV. Updating the differential for somatic and visceral inputs. JAOA, May;101(5):278-83, 2001
Korr I.M. The neural basis of the osteopathic lesion. JAOA, 47(4): 191-198, 1947
Korthuis RJ. Skeletal Muscle Circulation. San Rafael (CA), Morgan & Claypool Life Sciences, 2011
LeRoy R. Le vie du tissu conjonctif et sa defense par le massage. Rev. de Me. Paris, 58: 212, 1941
Schmidt R., Weidner C., Schmelz M. Time course of acetylcholine-induced activation of sympathetic efferents matches axon reflex sweating in humans. J Peripher Nerv Syst., 16(1): 30-36, 2011
Severini V., Venerando A. The physiological effects of massage on the cardiovascular system. Europe Medicophysica, 3:165-183, 1967
Szolcsanyi J. Neurogenic inflammation: reevaluation of axon reflex theory. In:Neurogenic Inflammation, Edited by Pierangelo Geppetti and Peter Holzer. ‘CRC Press’, 33-43, 1996
Valentine K.E. Masage in psychological medicine – modern use of an ancient art.New Zeland J. Physiotherapy, 12:15-16, 1984
Zabludovsky I.V. Massage Techniques. ‘Medicina’, St. Petersburg, 1913
Category: Medical Massage
