By Dr. Ross Turchaninov
We value our readers, their thoughts, opinions and contributions. This article is a great example of that. The idea to write it came to us as a result of an e-mail sent to Journal of Massage Science by Carole Clinch BA, BPHE who asked us to comment on the latest breakthrough in pain science.
There are a lot of misleading statements flowing in massage therapy since the profession tends to exist in its own little bubble, which is frequently detached from modern medical science. We understand that this article contains a lot of scientific data and info, but we think its subject is of great importance and we encourage readers to read this article all the way through. Otherwise they will continue to be fed partial truth about pain science.
SHORT HISTORY TRIP
Before we get to the actual topic of the article we need to take short history trip.
1. In 1965 Professors R. Melzack and P.D. Wall in the world’s most prestigious scientific publication, Science, published the Gate Control Theory of Pain which emphasized the role of the spinal cord’s gating mechanism in the formation of pain perception by the brain.
2. In 1990 Professor R. Melzack recognized that a further developed Gate Control Theory of Pain was needed. He introduced the Neuromatrix Theory of the Pain which showed the role the brain itself independently plays in the formation of pain perception in cases of phantom and chronic pains. To learn more about the Neuromatrix Theory please click here: https://www.scienceofmassage.com/2014/10/how-massage-heals-body-part-iv-phenomenon-of-pain-and-massage-therapy-neuromatrix-theory/
3. The main concepts of the Neuromatrix Theory of Pain were later picked up by Professor L. Moseley who deserves credit for spreading this theory in the medical community. However, Prof. L. Moseley generalized Neuromatrix Theory and used its concepts to explain the formation of pain perception in ALL clinical cases of pain. Such views seemed revolutionary at that time and created waves in the medical community and needed to be authenticated.
4. In 2012 a study was set up to examine the clinical outcome of Prof. L. Moseley’s views on the formation of pain perception to find out if indeed his treatment methods have clinical value when applied on actual patients. Prof. L. Moseley was invited as co-author of the study which tested his treatment techniques in the clinical setting.
The study examined the clinical effect of the Rubber Hand Illusion, which is the trademark of Prof. Moseley’s work. According to him this illusion is supposed to have impressive clinical benefits in the control of pain by addressing and altering the brain’s ability to form pain perception. We explain Prof. Moseley’s Rubber Hand Illusion at the end of this article:
Results of the study were published in 2012 (Mohan et al., 2012). Unfortunately, study showed that the treatment proposed by Prof. Moseley failed miserably in the clinical setting. Apparently, it is one thing to theorize in the lecture room and another to work on actual patients with pain. Here is the reference for this study where the name of Prof. Moseley as a co-author is in bold:
Mohan R, Jensen KB, Petkova VI, Dey A, Barnsley N, Ingvar M, McAuley JH, Moseley GL, Ehrsson HH. (2012). No Pain Relief with the Rubber Hand Illusion. PLoS One. 7(12):e52400.
And a final quote from the article:
“In two experiments, undertaken by independent research teams and both powered to detect a clinically relevant effect, we failed (bold by JMS) to detect any modulation of pain thresholds, nor of pain evoked by individually calibrated high and low painful stimuli, in association with the rubber hand illusion.”
MASSAGE THERAPY AND ‘NEW’ PAIN SCIENCE
Massage therapy alongside other health professions initially embraced the ‘new’ pain concept. However, this initial enthusiasm quickly faded for other health practitioners as soon as the independent study on the effect of the Rubber Hand Illusion, which we have referenced above, was published. This study confirmed that there are no widespread clinical benefits of pain management via the brain-only treatment approach, as it was suggested by Prof. Moseley. Despite this evidence, a vocal group of massage therapists continued to follow the same views and considered the ‘new’ concept of pain a breakthrough in pain science.
We observed that first hand since several years ago we were actively engaged in the discussion on this subject. To settle the ridiculousness of some therapists’ claims we contacted Prof. R. Melzack and asked for clarifications. Seeing direct danger to his legacy, Prof. Melzack gave an interview to the Journal of Massage Science despite that he retired from science and the last interview he gave was almost 10 years ago.
We published this interview in Issue #4, 2013 of JMS https://www.scienceofmassage.com/2013/10/persons-of-the-month-2013-issue-4/.
To our complete surprise same therapists claimed that we mislead Prof. Melzack with our questions. Until this day it is still puzzling for us how we were able to mislead a world-famous scientist with a set of simple questions.
So, where was the problem to start with? Prof. Melzack was the author of both theories and despite that they address different aspects of pain perception, the author insisted that they are two equally important components.
However, Prof. Moseley concentrated on the Neuromatrix Theory and suggested that ONLY the brain creates and modifies pain perception. For some of his followers the presence of the Gate Control Theory of Pain, which emphasized the critical importance of a gating mechanism in the spinal cord didn’t fit into this scenario. From this perspective, the only way to make things work in their favor was to proclaim that by introducing the Neuromatrix Theory of Pain Prof. Melzack denied his own Gate Control Theory of Pain, despite that in all publications he insisted that they complementarily worked with each other.
Before we move forward we would like the readers to take a pause for a second and read the following: If the Rubber Hand Illusion which was the trademark of the so-called ‘new’ pain science failed in the clinical setting and that failure was confirmed by independent study, how did it happen that the brain-only approach to somatic therapy still flourishes in the massage therapy community? Would you buy a car with new concept brakes if they failed in a crash test? We don’t think so but this is exactly what continues to happen in the massage therapy profession.
The new study published in the Journal of Clinical Investigation in May of 2017 puts everything in correct perspective and that is the main subject of this article.
THE IRREFUTABLE REBUTTAL TO THE ‘NEW’ PAIN SCIENCE
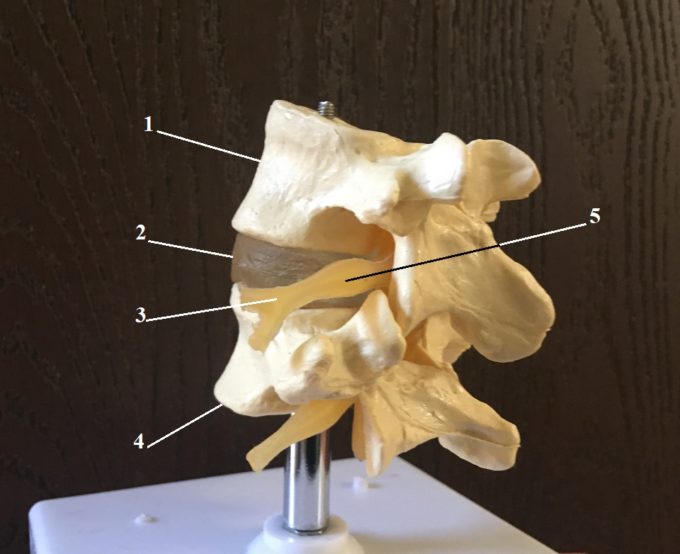
Before we get to the actual results of this breakthrough study of pain we need to quickly review the basics of neuroanatomy so readers can fully understand the value of the information the study uncovered. Fig. 1 illustrates the general view of the spinal segment.
Fig. 1. General view of the L4-L5 spinal segment
1 – L4 lumbar vertebra
2 – intervertebral disk
3 – L4 spinal nerve
4 – L5 lumbar vertebra
5 – dorsal root ganglion (DRG)
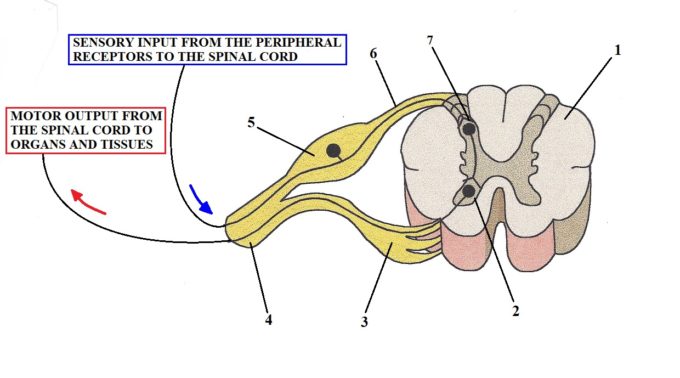
Fig. 2 illustrates the basic arrangement of the nervous system on the level of the spinal cord
Fig. 2. Basic arrangement of the nervous system on the level of the spinal cord
1 – Segment of the spinal cord
2 – Anterior horn (origin of motor response)
3 – Ventral root (motor commands going out)
4 – Spinal nerve
5 – Ventral root ganglion (DRG)
6 – Ventral root (sensory information going in)
7 – Posterior horn (sensory ‘computer’). This is also the location of Gates which modify pain perception on the level of the spinal cord as it was shown by Professor R. Melzack and P.D. Wall (1965)
Peripheral receptors, including nociceptors (i.e., receptors which detect harmful stimuli), located in the soft tissues and inner organs when activated deliver information in the form of the ascending sensory flow along the peripheral nerves and later spinal nerves to the segment of the spinal cord they are reporting to. These ascending sensory fibers split from their motor counterparts (which send motor response back to tissues and organs) just before entering the spinal cord, forming so called dorsal and ventral roots. The dorsal root carries only a sensory component to the spinal cord while ventral roots carry motor commands from the spinal cord to the areas where peripheral receptors were initially activated.
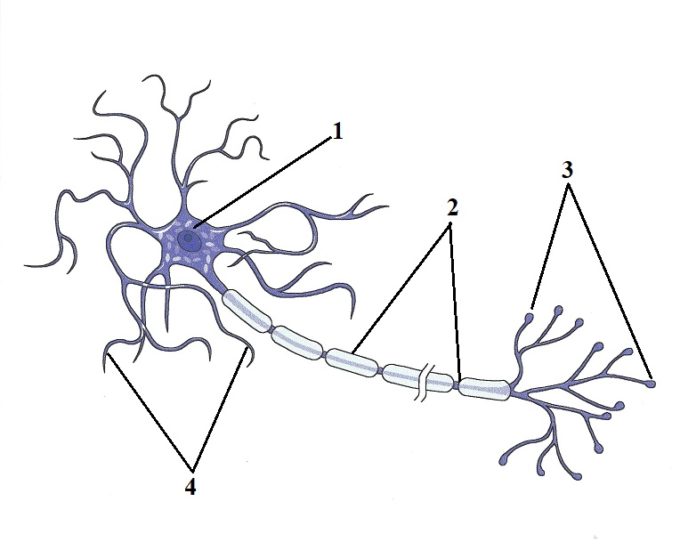
Each spinal and peripheral nerve consists of many neurons which carry information back and forth between soft tissues and inner organs and the central nervous system. Each neuron consists of three main components: dendrites, soma and axon. Fig. 3 illustrates the structure of the myelinated neuron.
Fig. 3. Structure of myelinated neuron
1 – soma or body of neuron located in dorsal root ganglion (DRG)
2 – axon (together axons form peripheral or cranial nerves)
3 – peripheral receptors in the soft tissue or inner organ
4 – dendrites
Soma – body of neuron
Dendrites – provide communication between bodies of neighboring neurons
Axon – long (sometimes several feet) projection of the neuron’s body. Combined axons form cranial or peripheral nerves, which like communication highways, connect CNS (brain and spinal cord) with organs and tissues.
Peripheral receptors – initial component of the neuron which detects any changes in the inner or outer environment
As soon as information from the receptors in the soft tissue and organs via the sensory part of the spinal nerve enters the spinal cord it meets with a sensory computer which analyzes the data and alters this data before sending it further up to the brain. This initial modification happens in the gates which are formed by special cells called subsantia gelatinosa and they are a critical part of the Gate Control Theory of Pain proposed by Professors Melzak and Wall in 1965. The presence of these gates kills ‘new’ pain science since it shows that other parts of the nervous system, besides the brain, modify sensory stimulation including nociception and thus alter pain perception before it reaches the brain.
Now let’s come back to Fig. 1 and Fig. 2 where you can see enlargement of the dorsal root called dorsal root ganglion (DRG). In this enlargement, all bodies of the neurons (see Fig. 3) which work with this particular segment of the spinal cord are located. It is ironic, but when I studied anatomy in Medical School I always thought that such large anatomical structures as DRGs must play a bigger role than just pure deposit of bodies of neurons.
In April of 2017 the Journal of Clinical Investigation published the results of a five-year study (Du et. al., 2017) conducted by an international group of scientists from USA, United Kingdom, China, Japan, and Malaysia. This study is considered a breakthrough in modern pain science and it still reverberates through the world medical community.
As we discussed the above, body of neurons tightly packed together in the DRGs and as shown in Fig. 2 have short projections called dendrites. For years it was known that dendrites inside of DRGs besides holding bodies of neurons together, have receptors which work with the same neurotransmitters which control the nociception (i.e., formation of pain perception) on the level of the brain. However, no one before the authors of this study asked the very simple question: Why do neurons in DRGs located outside of the CNS carry the SAME receptors and neurotransmitters which are used by the brain to form pain perception (i.e., nociception)? Thus, the initial intention of this study was to find the answer to this question.
The authors conducted a series of brilliant experiments which examined functions of DRGs. Here is a short description of one of them. The micro cannula was inserted into DRG of experimental animals (rats) and it delivered a small dosage of neurotransmitter GABA inside of DRG. GABA is a major inhibitory neurotransmitter within the CNS which suppresses the pain analyzing system and it also decreases tone in the skeletal muscles. As we mentioned above, it was known before that dendrites of the body of neurons located in DRG carry GABA-receptors.
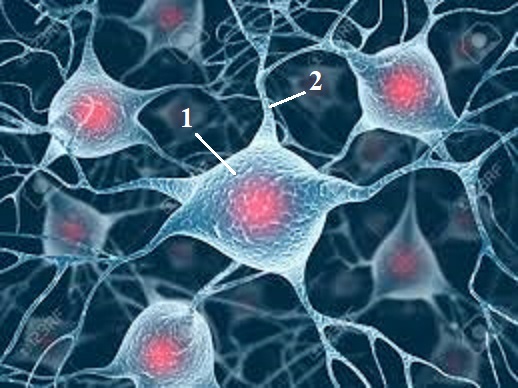
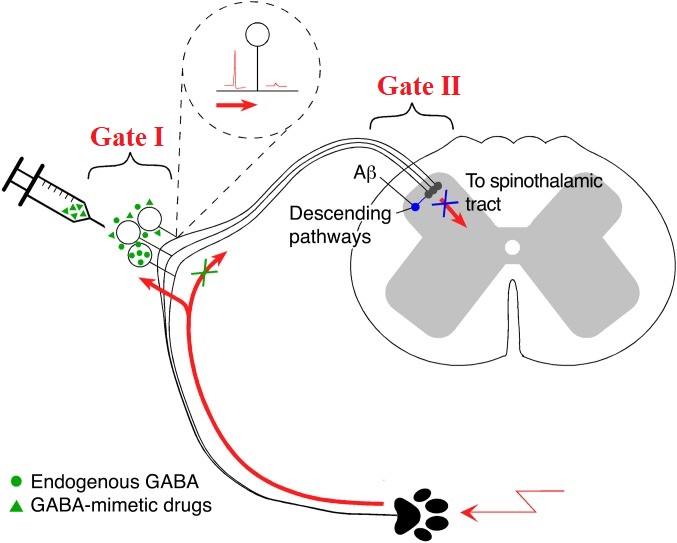
After insertion of cannula and adding GABA into DRG the authors injected in the rat’s hind paw noxious substances which normally trigger intense pain reaction. However, externally injected GABA dramatically decreased the formation of pain perception after noxious substances where injected into the paw. If, just saline was injected into DRG it didn’t modify pain perception and the animals exhibited intense pain reaction to injection of irritable substances. There are several other experiments conducted by the authors to check and double check their initial findings. Eventually they concluded that DRGs are Gate I which modulates nociception and alters pain perception OUTSIDE of the CNS. To do that efficiently, a body of neurons located in DRG communicate and work together via their dendrites IN THE SAME WAY as neurons work and communicate within the brain itself. Fig. 4 illustrates bodies of neurons and their communications via dendrites.
Fig. 4. Network of neurons communicating via dendrites
1 – body of neuron
2 – dendrite
Thus, each DRG works as a small brain (this term was coined by Prof. N. Gamper, one of study’s lead researchers), which alters initial sensory information especially nociception while letting into the CNS only the information which is needed to be delivered to the brain. In such case the brain becomes more receiver that actual producer of pain perception! In other words, the brain receives already modified and altered nociception and it transfers it to our consciousness. Thus, the brain plays a lesser role in formation of pain perception, compared to what we thought it did, before this study was published.
Of course, according to the Neuromatrix Theory of Pain, the brain can also independently generate pain perception – for example, in cases of phantom or psychosomatic pains. However, even in this case the constant replication of pain perception by the brain still relied on initial activation of nociceptors and further modulation of pain perception in the Gate I (DRG) and Gate II (posterior horn of the spinal cord) BEFORE these stimuli even reached the brain.
The results of this study triggered earthquakes among pain scientists and physicians around the world since it opened completely new horizons in the future clinical application of its findings. The therapy which will target nociception on the level of DRGs without the brain itself may become the only way to stop the opioid epidemic, which kills 50,000 people each year in the USA alone.
All these people continue to die because of the dominance of the false notion that to control pain we need to target the brain itself, since this is the where pain perception modulates and forms. Technically speaking, these are the same false ideas which continue to be spread within the massage community about formation and treatment of pain. This is why this breakthrough study has such importance for everyone who is trying to address various somatic and visceral pains.
We followed reactions of therapists to this recent study and we noticed that some are incorrectly reading its results. Some therapists believed that this new gate introduced by Du et. al., (2017) denied the presence of gates described by Prof. Melzack and Wall which are located inside the spinal cord in the posterior horns (see Fig. 2). However, this is a completely incorrect reading since the authors of this study specifically mentioned that their work didn’t cancel or diminish the role of initial gates introduced by Professors Melzack and Wall in 1965:
“Thus, our study proposes an additional (bold by JMS) mechanism to the broadly accepted Gate Control Theory of Pain, which postulated that integration of ascending peripheral and descending central pathways in the superficial dorsal horn can “gate” nociception.”
Du et al., (2017)
The only difference is that Du et. al., (2017) suggested labeling DRG as Gate I and substantia gelatinosa as Gate II. In Fig. 5 we used the illustration from the original article where Gate I and Gate II are in the red font.
Fig. 5. New arrangement of Gates I and II proposed by Du et. al., (2017)
IMPACT OF STUDY ON ‘NEW’ PAIN CONCEPT AND MASSAGE THERAPY
This study is an exceptional piece of science which puts everything in correct perspective. As we now know formation of pain perception is not the prerogative of the brain only. The spinal cord (Gate II) alters it and even such structures as DRGs which don’t even belong to the CNS, are greatly altered and modify pain perception.
Thus, this study offers air tight proof that pain perception is a very complex event and many components including the brain itself pay an equally important role in pain formation.
Unfortunately, a group of therapists still follows the false notion that the brain is the only place where pain perception is formed and modified and their views still circulate and mislead other therapists in the field.
We’ve waited until the end of this article to explain our views on Prof. Moseley’s work and to the work of his followers in massage therapy. We don’t want readers to get the sense that we consider them completely wrong. The ideas of Prof. Melzack’s Neuromatrix Theory which Prof. Moseley spreads are absolutely correct. The major difference is that Prof. Melzack used Neuromatrix Theory to explain formation of pain in specific cases while Prof. Moseley and his followers in MT incorrectly generalized Neuromatrix Theory in all cases of somatic pain.
Secondly, followers of Prof. Moseley’s work in the massage therapy profession introduced a new treatment option called Dermoneuromodulation. This treatment option is completely correct but what is incorrect that it was promoted to therapists as the ultimate clinical solution to all cases of somatic pain.
We reviewed the technical arsenal of Dermoneuromodulation and with 100% assurance we can testify that working with skin and stretching peripheral nerves are indeed very effective clinical tools. Our students around the county are using these techniques on a daily basis. However, they are only the components of somatic rehabilitation since the other three equally important types of soft tissues with their own peripheral receptors (connective tissue, skeletal muscles and periosteum) MUST be evaluated and addressed as well.
As a final note – techniques advocated by Dermoneuromodulation have been known and used in somatic rehabilitation for more than100 years. Actually, they were the first stepping stones in the development of the modern Medical Massage concept. The exactly similar to Dermoneuromodulation’s techniques were successfully used within the areas of cutaneous reflex zones called Head’s Zones as far in the past as 1903 (Professor A.E. Sherbak). We strongly believe that re-naming already existing therapies and fragmenting the bigger picture of the integrative approach to somatic rehabilitation jeopardizes future development of the clinical wing of the massage therapy profession and its eventual incorporation into modern medicine where it was successfully used in the past.
We consider study we reviewed in this article of such importance that we ask our readers to share this article or original study with as many therapists as possible to stop confusion while practice and promote pain science based on data rather than personal opinions.
REFERENCES
Du X, Hao H, Yang Y, Huang S, Wang C, Gigout S, Ramli R, Li X, Jaworska E, Edwards I, Deuchars J, Yanagawa Y, Qi J, Guan B, Jaffe DB, Zhang H, Gamper N. Local GABAergic signaling within sensory ganglia controls peripheral nociceptive transmission. J Clinical Invest., (2017) May 1; 127(5): 1741–1756.
Sherbak A.E. (1903) Further Experimental Studies of Physiological Effects of Mechanical Oscillations. Physiology Review, 9: 641-649 and 10: 722-733.
Melzack R. (1990) Phantom Limbs and The Concept of Neuromatrix. Trend Neurosci., 13:88-92.
Melzack, R., Wall, P. (1965) Pain Mechanism: A New Theory. Science, 150(Nov): 971-979.
Mohan R, Jensen KB, Petkova VI, Dey A, Barnsley N, Ingvar M, McAuley JH, Moseley GL, Ehrsson HH. (2012). No Pain Relief with the Rubber Hand Illusion. PLoS One. 7(12):e52400.
Category: Medical Massage
Tags: 2017 Issue #3