By Dr. Ross Turchaninov, MD
Despite a mountain of studies, publications and countless CEU classes, hypertonic muscle abnormalities, especially active Trigger Points (TP), continue to affect patients’ lives, devastate communities with an opioid crisis while driving up cost of medicine. 31 million Americans suffer from low back pain at any given time (N Engl J Med. 1994) while according to the CDC, only 15 million Americans suffer from COPD.
JMS has already extensively covered the topic of TPs and their formation. In the first issues of JMS in 2009 we published a two-part article, “Science of Trigger Point Therapy:
Part 1: https://www.scienceofmassage.com/2009/03/science-of-trigger-point-therapy-part-i/
Part 2: https://www.scienceofmassage.com/2009/05/issue-3-2009-contents/
We continued the discussion about the clinical value of ischemic compression as a main clinical tool to address local vasoconstriction in 2011 in the article: “Ischemic Compression: To Be Or Not To Be? Science of Trigger Point Therapy”: https://www.scienceofmassage.com/2011/10/ischemic-compression-to-be-or-not-to-be-science-of-trigger-point-therapy/
Finally, in 2018 JMS published in two parts an important article about neuromuscular junctions and their role in formation of TPs: “Let’s Talk About Neuromuscular Junctions”
Part 1: https://www.scienceofmassage.com/2018/01/lets-talk-about-neuromuscular-junctions-part-i/
Part 2: https://www.scienceofmassage.com/2018/05/lets-talk-about-neuromuscular-junctions-part-ii-evaluation/
.
In this article we would like to revisit this important topic using new scientific data about TPs. We will also discuss very common misunderstandings of the trigger point concept as well as their correct and incorrect treatment options.
FIRST RECORDED IMAGE OF ACTIVE TRIGGER POINT
Until 2007 medical science did not have any reliable proof of TPs existence. Their presence was confirmed strictly on the patients’ complaints, local palpations skills by the examiner and registration of muscle impaired function. These widely used clinical tools are very important, but extremely subjective and they carry little weight in medical science.
If we relied strictly only on these subjective proofs the counterargument that somatic pain in the form of TP is pure patient brain’s creation had a point. What additionally compromised TPs concept is the fact that despite all treatment options (TPT, stretchings, injections, acupuncture, etc.) tend to come back and bother patients again.
No, blood test, X-ray, electromyography etc. were able to prove that TP is a structural change in the muscle itself. Even an MRI failed to detect the presence of active TPs and it got to the point that some scientists started to see TPs as a pain pattern developed by the brain as its response to trauma or chronic overload rather than actual pathological changes inside the muscle tissue itself. These wrongful views eventually culminated in so-called ‘new pain science’ and they unfortunately got a second life among therapists who are not aware of recent developments in the science of somatic medicine and were simply misguided by unscientific claims.
In 2007 a breakthrough study was published in Archives of Physical Medical Rehabilitation (Chen et al., 2007). The newly developed diagnostic modality called magnetic resonance elastography decisively proved that TPs are structural changes in the myofibrils rather than simple pain pattern developed in the brain without any local abnormalities in the affected muscle.
Fig. 1 from the original study is first recorded by the medical science image of active trigger point. It illustrates the structure of myofibrils inside the normally functioned trapezius muscle (a) and myofibrils inside the active TP developed in the hypertonically changed trapezius muscle (b).
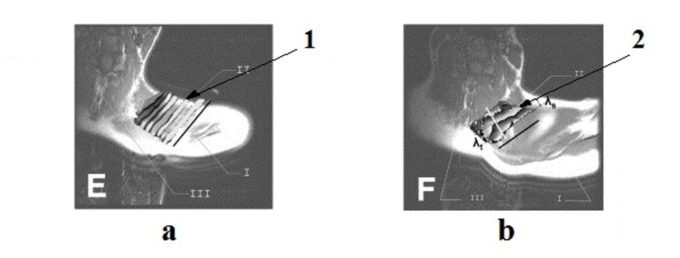
Fig. 1. Magnetic resonance elastography of the normal and affected trapezius muscles
(Chen et al., 2007)
a – healthy trapezius muscle
b – trapezius muscle with active TP
By comparing both pictures it is obvious that myofibrils inside of active TP (Fig. 1 b ‘2’) are swollen and twisted and these structural changes are responsible for the clinical symptoms of pain and dysfunction. Of course, pain and other pathological symptoms are produced by the brain, but they are based on the data obtained from the peripheral receptors located in the affected muscles. This study finally put to rest unscientific speculations that pain due to trigger point presence is pure brain product without any local changes being the initial cause of it.
Before his unfortunate death Dr. Simmons (2008) applauded the result of this study since he witnessed firsthand that his and Dr. Travel’s work was finally justified, and their predictions indeed are supported by modern science. Right now, the presence of structural changes inside of active TP is an undoubtedly proven fact. Please completely disregard classes or publications which suggest otherwise. They are unscientific claims whose only goal is to simply confuse therapists!
NEUROLOGICAL ORIGIN OF ACTIVE TRIGGER POINTS
Education of therapists and chiropractors generation after generation was based on the same notion that active TPs in the skeletal muscles are areas of local ischemia which need to be treated locally in order to eliminate vasoconstriction and restore proper oxygenation of the tissue. It seems that it is a simple and elegant concept. Of course, there are other factors suggested as well (ATP depletion, various histochemical reactions, etc.), but we still can identify this basis concept as a core view of TP concept and its treatment options.
We would like readers to pause for a second and think how many of us around the world conduct therapy based on this principle. There is always a new class or publication which promises complete elimination of TPs and we run for it hoping that real answer is finally here!
If suggested therapies are correct ones, then the conducted treatment MUST guarantee stability of its results and there is no need for endless ’new’ classes or publications.
Unfortunately, that is not the case. It seems that TPs have the tendency to return and frequently therapists are facing them again and again in the same patient. Thus, something is fundamentally wrong with our basic understanding of hypertonic muscular abnormalities in general and active TPs in particular. If the theory behind the therapy is incorrect then therapy itself is destined to fail.
The first attempt to examine and treat active TPs was done by German physician Froriep in 1843. However, the real fathers of our understanding of TP formations are Dr. H. Shade from Germany and Dr. J. Mackenzie from the United Kingdom. Besides formulating the entire concept of hypertonic muscular abnormalities they defined its three forms as hypertonus, trigger point and myogelosis.
They also put forward another very important aspect of TP’s theory. They both clearly pointed to the neurological origin of TPs formation if they weren’t developed as a result of trauma. Thus, Shade and Mackenzie identified active TPs as a reflex reaction of the muscles to the mild to moderate irritation of the motor part of the spinal or peripheral nerve or motor nerve itself. All these neurological structures are directly responsible for the motor innervation of the muscle.
The excellent textbook Trigger Point Manual written by Dr. Travel and Dr. Simmons made one mistake – the authors almost completely dropped from the textbook even the possibility of TPs being reflex reaction of the muscle to the compromised motor innervation. However, in clinical reality the mild to moderate irritation of the spinal, peripheral or motor nerve, which are responsible for the innervation of muscles, are real causes of TPs formation in the majority of cases. Unfortunately, this critically important piece of medical science is for generations absent even in basic education.
Dr. Simmons at the end of his life started to see value in the Dr. Shade and Dr. Mackenzie position. He greatly contributed to science of TP by showing that compression and irritation of the motor nerve inside neuromuscular junctions (NMJ) are important mechanism in TPs formation (Simmons et al., 2002). We discussed the importance of NMJs for TP concept in the two-part article mentioned above and we suggest readers review this important data.
Despite that recognition of the pressure on NMJs’ as one of mechanisms in TPTs formation is important, it is not going far enough. If we look at tension around each NMJ as the only cause of TPTs formation, we continue to talk about locality of events since NMJs are located in the middle of muscle belly where the motor nerve gets in touch with muscle tissue. Thus, we may continue to see TPs as local events instead of their formation as a reflex reaction.
Considering the wide spread of muscle hypertonicity and TPs among the patients, as well as their resilience to the therapy more scientists look back on the original theory of TPs formation which emphasized its neurological nature and pointing to the TPs being pure reflex reaction. In such case active TPs are seeing as a reflex response of the muscle, which harbors them, to the pathological changes sometimes located in completely different part of the body (Sihvonen et al., 1995; Dubuisson et al., 2001).
Since the patient is not mentioning that area in his or her complains everyone are treating TPs and local event, where the TP is located, while the real cause silently sits in a completely different area which looks unrelated to the current symptoms. Let’s discuss one of recent studies which is a great illustration of Dr. Shade and Dr. Mackenzie being correct.
As we know one of the major sources of the trapezius muscle’s innervation is the assessory nerve (AN). AN is a very weird nerve. Generally speaking, we can split all our nerves in two large families: cranial nerves and spinal nerves. Cranial nerves originate from the brain itself while spinal nerves originate from the spinal cord. For example, the vagus nerve which is the main control of our inner organs is cranial nerve while sciatic nerve is an extension of the lumbar spinal nerves. AN is weird because of its unusual anatomy and pathway. Fig. 2 illustrates pathway of AN.
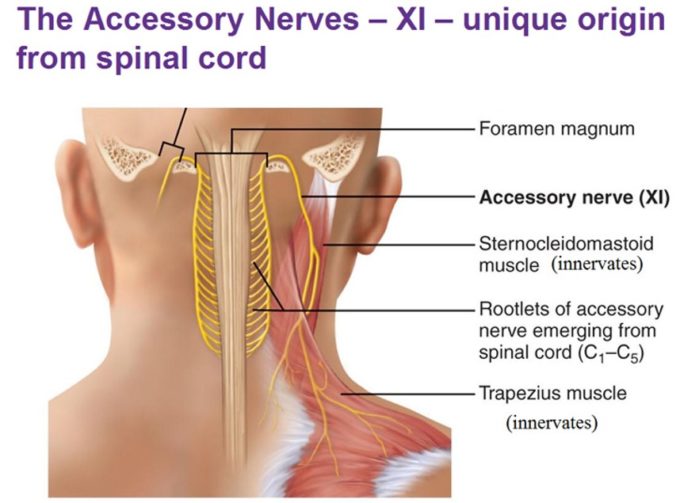
Fig. 2. Pathway of accessory nerve (AN)
AN originates from small rootlets of C1-C5 which when united form the trunk of the nerve. It then ascends up and together with the spinal cord enters the skull through its major opening -foramen magnum. It continues inside on the skull until it leaves the skull together with vagus nerve via jugular foramen. While vagus goes down AN goes down and curves backward providing innervation of the trapezius and sternocleidomastoid muscles. Thus, AN is not pure cranial nerve, but rather spinal nerve which takes an intracranial pathway. However, the presence of the intracranial segment gives AN the right to be called cranial nerve #11.
In 2015 a group of scientists (Akamatsu, et al., 2015) conducted cadaver study when they examined correlations between location of the main active TPs in the trapezius muscle with the pathway of AN. Fig. 3 illustrates study results.
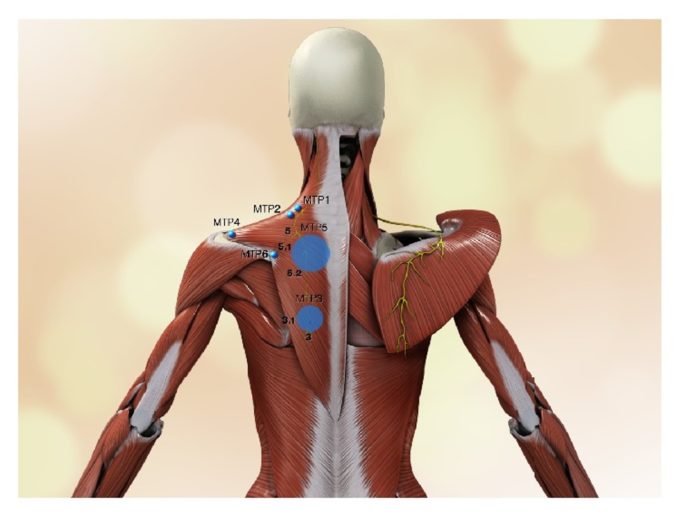
Fig. 3. Relations between assessory nerve and location of active TPs
Let’s go over the image. On the left, the trapezius muscle is intact while on the right side it is cut and rolled to the side to expose the pathway of AN indicated in yellow. On the left side you may also see the pathway of the AN but as a yellow shadow seen through the fibers of the trapezius muscle. Also, on the left side the authors of the study indicated the location of the main active TPs by blue circles. Larger circles indicate more frequent clinical cases of active TPs, smaller circles less frequent clinical significance. As it is clearly seen on the left side all major active TPs follow the exact pathway of AN. This study is a great visual illustration of the fact that active TPs formation has clear neurological origin and it is first of all a reflex reaction of the muscle to the compromised innervation.
Let’s now follow the pathway of AN in Fig. 2. As you can see the AN can be affected by the tension in different somatic structures while it tries to get to trapezius and sternocleidomastoid muscles. Tension in trapezius itself may affect AN especially in the places where it forms NMJs with myofibrils. Dr. Simmons pointed to this mechanism of tension.
However, if spenius capitis, levator scapulae and scalene muscles are tense they may mildly irritate AN and clinically the therapist will see it as pain and dysfunction of the trapezius muscle while the real problem is tension in completely different somatic structures.
Let’s look at the situation from a clinical perspective. If scalene muscles irritate AN and tension in the trapezius is formed as a reflex reaction, any therapy applied to the trapezius itself (TPT, MET, acupuncture, dry needling etc.) becomes an endless waste of time, effort and patient’s or insurance money. In such case the treatment must be applied on the lateral and anterior neck to decompress scalene muscles rather than patching a local problem in trapezius.
Thus, in the case of TPs being reflex zones the chain of events are the following: mild irritation of the motor fibers of the spinal or peripheral nerve or motor nerve itself → increase in resting muscle tone → slight decrease of blood perfusion first of all at night → formation of local ischemia with secondary structural changes in the myofibrils themselves → TP formation → various consequences such as ATP depletion, histochemical reaction etc.
Thus, since the current theoretical model failed to deliver a stable clinical result, we need to come back to the original theory proposed by Dr. Shade and Dr. Mackenzie as this and other recent studies indicated. However, for that to work in a clinical setting the therapists must completely change the treatment strategy.
For a therapist to help patient, he or she must first identify the presence of all possible sites where the spinal or peripheral nerves can be irritated starting from the intervertebral disk all the way down to the NMJs. Without that critical piece of data locally conducted therapy in the form of TP Therapy, various corrections of structural misalignments or even Muscle Energy Techniques become an endless chase of our own tails. Only when the fact of reflex zones absence is clearly established the therapist has professional rights to treat TP with local therapies. If the therapist even suspects the presence of reflex mechanism of TP’s formation the entire treatment strategy must be changed, and therapy must target the initial trigger first.
If therapists continue to approach treatment of TPs as well as other hypertonic muscle abnormalities only from the perspective of local changes, they will continue to patch the problem rather than decisively eliminate it. In the Part II we will discuss circulatory changes in the area of active Trigger Point.
REFERENCES
Akamatsu F.E., Ayres B.R, Saleh S.O., Hojaij F., Andrade M., Hsing W.T., Jacomo A.L. Trigger Points: An Anatomical Substratum. Biomed Res Int. 2015; 2015: 623287.
Chen, Q., Bensamoun, S., Basford, J.R., Thompson, J.M., An, K.N. Identification and quantification of myofascial taut bands with magnetic resonance elastography. Arch Phys Med Rehabil. 2007; 88: 1658–1661.
Dubuisson A, Foidart-Dessalle M, Cohnen A, Zeimetz C. [Thoracic outlet syndrome]. Rev Med Liege. 2001 Feb;56(2):97-105.
Froriep R. Ein Beitag zur Pathologie und Therapie des Rheumathismus. Weimar, 1843
Mackenzie J., Angina Pectoris. Henry, Frowde & Stroughton, London, 1923
Schade H. Untersuchungen in der Erkaltungstrade: III Uber den Rheumatismus, in besondere den Muskelrheumatismus (Myogelose). Munch Med Wschr 68, 95-99, 1921
Sihvonen T, Lindgren KA, Airaksinen O, Leino E, Partanen J, Hänninen O. Dorsal ramus irritation associated with recurrent low back pain and its relief with local anesthetic or training therapy. J Spinal Disord. 1995 Feb;8(1):8-14.
Simons D.G. New views of myofascial trigger points: etiology and diagnosis. Arch Phys Med Rehabil. 2008 Jan;89(1):157-9.
Simons D.G., Hong C.Z., Simons L.S. Endplate potentials are common to midfiber myofacial trigger points. Am J Phys Med Rehabil. 2002 Mar;81(3):212-22.
Travell, J .G.,Simons, D.G.: Myofascial Pain and Dysfunction. The Trigger Points Manual. “Williams & Wilkins, Baltimore, 1983.
Category: Medical Massage
Tags: 2019 Issue #4
