By Dr. Ross Turchaninov, Phoenix, AZ
We started discussion about new scientific data regarding active Trigger Points (TP) in the previous issue of JMS: https://www.scienceofmassage.com/2019/12/new-scientific-data-to-revisit-active-trigger-points-concept-part-i/
The subject of this article is circulatory changes registered in active TP. Despite the obviousness of this topic its importance is greatly misunderstood and mispresented. It is very well documented that various structural changes in combination with other factors (e.g., irritation of the motor nerve, increase in the sympathetic tone etc.) trigger local vasoconstriction and ischemia, starting the process of TP formation.
It is the therapist’s job to remove local vasoconstriction, restore normal circulation and eventually eliminate local ischemia and active TP. It can be done decisively only when the therapist combines local and reflex mechanisms of massage therapy reestablishing proper oxygenation of the myofibrils while restoring normal anatomical length of the affected muscle.
One of the important clinical tools is Trigger Point Therapy (TPT) which uses ischemic compression to trigger reflex vasodilation. We have already discussed topic of TPT in previous issues of JMS:
Part 1: https://www.scienceofmassage.com/2009/03/science-of-trigger-point-therapy-part-i/
Part 2: https://www.scienceofmassage.com/2009/05/issue-3-2009-contents/
In this article we would like to concentrate on the phenomenon of local ischemia itself. In any textbook on somatic rehabilitation, the topic of TP and TPT discussed in details and location of active TPs in various muscles is well presented. All widely used TPs charts provide same information and all these sources correctly guide the therapists to identify and isolate active TP during the tissue evaluation. However, a majority of therapists got the wrong impression that TP is an actual ‘point’ inside the affected muscle, and it needs to be treated accordingly, i.e., pinpoint location inside the muscle as it is presented in the charts or textbooks.
Clinical reality is much more complex since ‘point’ which indicates the location of active TP, is only the epicenter of local ischemia while the area with local vasospasm is much larger than TP presented as a ‘dot’ in any textbook or chart.
If therapists approach the treatment of TP from the ‘point’ perspective only, it greatly diminishes clinical effectiveness of the therapy since the entire area of ischemia was never fully addressed. That is one of the contributing factors in the formation of so-called latent TP with following re-emergence of active TP in the same area.
Let’s look at results of one interesting study, which used thermography to examine the area of active TP located in the levator scapulae muscle, from the perspective of local ischemia affecting all tissues rather than the muscle itself (Magalhães et al., 2015).
Thermography is detection in fluctuations in the skin’s temperature using a thermographer. If, for any reason the local vasoconstriction in the skin developed it is going to decrease arterial blood supply and local temperature falls. If there is increase in the arterial blood supply or delay in drainage from the skin the local temperature is rising and even its slightest increase is going to be registered by very sensitive thermographer which detects and records even the slightest fluctuations in the skin’s temperature. The decrease of the local temperature the thermographer records all way to whiteness while the increase of circulation is recorded as a bright red.
Firstly, the authors of this study clinically detected the presence of active TP in the levator scapulae muscle based on the patient’s complaints and local evaluation of soft tissues. Next, they placed markers around the tested area and after that the thermography was performed to register fluctuations in the local temperature in the upper shoulder and back. Fig. 1 illustrates results of the study.
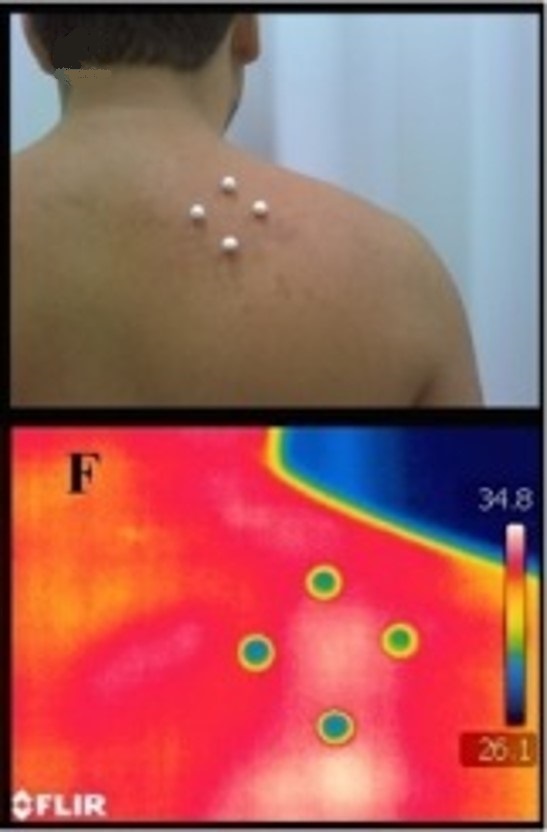
Fig. 1. Thermography to skin’s ischemia in cases of active TP in levator scapulae muscle (Magalhães et al., 2015).
C – markers on the skin around active TP
F – thermogram of the skin with markers
Before we move forward let’s shortly review the anatomy of the area. That is very important and relevant for future discussion since there are 4 layers of soft tissue located above the levator scapulae muscle: skin with subcutaneous tissue, superficial fascia (it covers the trapezius m.), trapezius muscle and middle fascia (separates trapezius m. from levator scapulae m.).
Let’s now read the thermogram together (see Fig. 2).
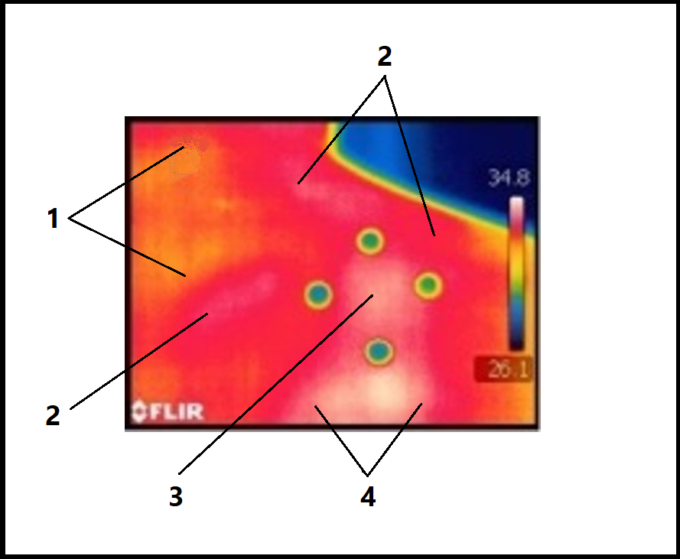
Fig. 2. Thermogram of the right shoulder with active TP in levator scapulae muscle (Magalhães et al., 2015)
1 – area of normal circulation
2 – arterial blood depot
3 – skin ischemia in the area of active TP
4 – skin ischemia outside of the area of active TP
We would like readers to examine these three areas in the thermogram:
Skin Ischemia
All subjects had active TPs which were detected in their levator scapulae muscles. However, the thermography examines the circulation in the skin only by detecting the fluctuation in the local temperature. If a reader looks at the thermogram of the right scapula the white area of vasoconstriction is clearly visible between markers because decrease of the skin’s blood supply the thermographer registers as an area of whiteness or lower temperature (see Fig. 2 ‘3’and ‘4’).
There are two important observation from the thermogram:
1. The active TP in the levator scapulae triggers active vasoconstriction all way to the skin despite that affected muscle is in the 5th layer of the soft tissues. If we can clearly register local ischemia in the skin it means that the same or even greater ischemia developed also in the underlying layers of the soft tissues (fascia and trapezius muscle) which cover the levator.
Meaning: The local vasoconstriction in the small area of active TP located in the very deep layer of the soft tissues ALWAYS triggers reflex vasoconstriction in all layers of the surrounding soft tissues.
2. The thermogram illustrates another interesting finding. Fig. 3 illustrates the commonly accepted location of the lower active TP in the levator scapulae. The therapist may find it in any textbook or diagram.
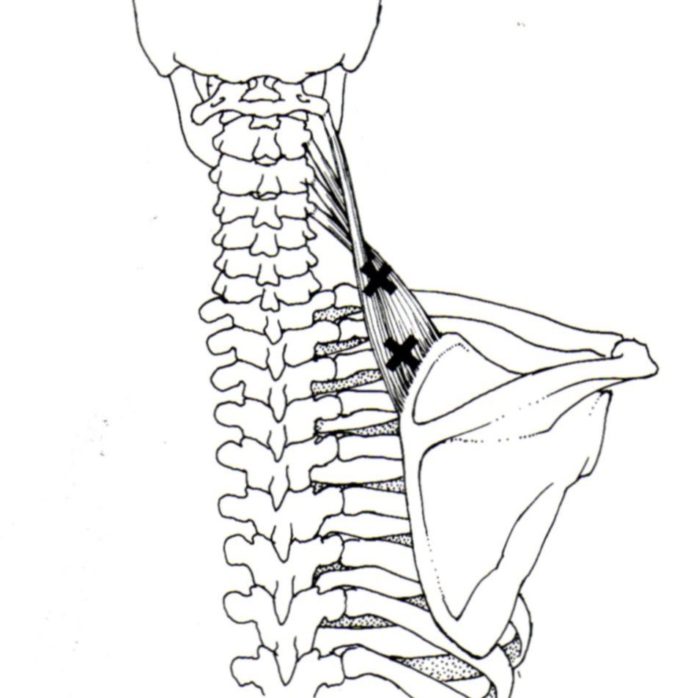
Fig. 3. Location of the lower active TP in the levator scapulae muscle (Travel and Simmons, 1983).
As you can see in Fig. 3, the active TP in the levator scapulae muscle, which was tested in the study, is above the upper medial angle of the scapulae and that area is in the middle of the markers which were placed on each subject before thermography was performed (see Fig. 1 ‘C’).
However, if we compare the location of active TP in the levator scapulae muscle with results of thermography (see Fig. 2, ‘4’) it is obvious that this area of skin vasoconstriction and ischemia in thermogram extended all way down below the markers placed to mark the area of active TP location. Thus, it is obvious the area of vasoconstriction (whiteness) in the thermogram is many times larger than the actual size of active TP in the levator scapulae muscle.
Meaning: Why is the area of the vasoconstriction extended all the way down beyond markers which were placed on the skin before examination of local circulation? Such extension of local vasoconstriction reflects the impact the force of gravity has on circulation since the area of vasoconstriction is never restricted to the active TP itself, but it is going to always negatively affect circulation in the underlying soft tissues according to the direction of gravity’s pull. Since the patient was standing during thermography the gravity was directed inferiorly and it enhanced local vasoconstriction in this direction.
Arterial Blood Depot
Around the area of local ischemia, the skin is bright red (see Fig. 2 ‘2‘) and it means that the temperature of the skin is higher than normal. What we observe is the body’s desperate attempts to eliminate vasoconstriction in the skin and in all layers of the soft tissues triggered by presence of active TP.
After chemoreceptors in the area of ischemia detected a decrease of oxygenation the body immediately reacted by creating peripheral vasodilation AROUND the area of vasoconstriction. This phenomenon is called blood depot and it is clearly registered by a thermographer as an increase in the local temperature around the area of witness (local ischemia).
Meaning: As long as the area of ischemia is present (in this case in the skin) the body is going to constantly fight with it through the deliverance of extra blood around it, forming a blood depot. Thus, blood which is needed for the oxygenation is available, but local vasoconstriction is not permitting it get into the area affected by the ischemia.
Area of Normal Circulation
The parts of the body with normal circulation are seen on the thermogram in yellow color (see Fig. 2, ‘1’). As a result of successful Medical Massage therapy which should include TPT with the consequent application of Muscle Energy Techniques, the area of local ischemia in the muscle as well as in all layers of the soft tissues including skin is eliminated. When that happens, the thermograph is going to register normal temperature of the skin in the upper shoulder and the examiner is going to observe it as yellow color on the thermogram.
Circulation And Clinical Application Of The Massage Therapy
The goal of MT is to eliminate local ischemia in all layers of the soft tissues and restore normal circulation by triggering local vasodilation. As readers saw in Fig. 1 and 2 the local ischemia in cases of active TPs never was restricted to the muscle itself. Thus, the necessity of therapy which targets the area of TP only is a widely circulated mistake.
If the therapist would like to decisively eliminate active TP instead of putting it into a ‘sleeping’ state, he or she must see the larger clinical picture and target the soft tissues on a layer by layer basis, eliminating the condition of the local ischemia in each layer separately, including of course, the levator scapulae muscle which harbored the initial TP.
Finally, while developing treatment plan the therapist must consider the impact of the force of gravity on the circulation in the soft tissues since the area of local ischemia always extends from the area of active TP in the direction of the gravity pull and that factor must be considered when treatment protocol is formulated.
For further references we discussed scientific data on how MT triggers local vasodilation using local and reflex mechanisms in a two parts article on mechanisms MT uses to promote vasodilation in the soft tissues:
HOW MASSAGE THERAPY HEALS THE BODY. PART III: Vasodilation Mechanisms
HOW MASSAGE THERAPY HEALS THE BODY. PART III: Vasodilation Mechanisms
CONCLUSION
Various publications, educational seminars, webinars, etc. which cover hypertonic muscular abnormalities in the form of active TPs, continue to present this topic as a muscle pathology. However, clinical reality is much more complex and such a one-sided view, while bringing temporary relief for the patients, diminishes clinical outcomes of the therapy. It acts as a temporary patch which requires revisiting the same issue again and again.
The study results we reviewed in this article examined the relations between active TP located in the deeper muscle layer (levator scapulae muscle) and area of skin which is not even in direct contact with that muscle. However, exactly the same relations exist between the levator scapulae muscle and fascia which covers the upper portion of the trapezius muscle or between the levator scapulae muscle and periosteum of the scapula itself. These relations which are called reflex zones are mediated by the peripheral nervous system via so called soma-somatic reflexes.
Disregarding reflex zones examination and their elimination is a clinical mistake since only a comprehensive approach to the treatment of active TPs can provide relatively quick and stable clinical results. There is no doubt that there are pathological changes in the myofibrils involved in active TP. At the same time, these changes are only part of the clinical reality. Thus, the notion that active TPs are solely muscular abnormalities must be abandoned once and for all if we consider patients’ interests as a priority.
Let’s review the clinical situation with the active TP in the levator scapulae muscle. So, the therapist correctly identified its presence based on various charts and textbooks. He or she also used completely legitimate and clinically valuable tools (Trigger Point Therapy, Muscle Energy Techniques etc.) to eliminate hypertonicity. However, his therapy targeted the muscle in the area suggested by the cart or textbook. By doing that the therapist makes a critical mistake since only one aspect of the complex clinical picture now addressed. Such a one-sided approach to the therapy will never deliver stable clinical results, especially in complex chronic cases while it indeed is going to provide temporary relief.
Thus, therapists must see the larger picture since active TP is only part of the puzzle rather than the puzzle itself. Having such vision and practicing it correctly equals an integrative approach to somatic rehabilitation. In such case all four types of the soft tissues (skin, fascia, muscles and periosteum) are examined and treated on a layer by layer basis with customized treatment strategy which includes Trigger Point Therapy, but is not limited to it, since other modalities targeting all types of the soft tissues are also used.
REFERENCES
Magalhães MF, Dibai-Filho AV, de Oliveira Guirro EC, Girasol CE, de Oliveira AK, Dias FR, Guirro RR. Evolution of Skin Temperature after the Application of Compressive Forces on Tendon, Muscle and Myofascial Trigger Point. PLoS One. 2015.
Travel J.G., Simmons D.G. Myofascial Pain and Dysfunction. The Trigger Point Manual. Williams&Wilkins, 1983
Category: Medical Massage
Tags: 2020 Issue #1
