by Dr. Ross Turchaninov
This article finalizes our ongoing discussion on the formation of reflex zones in soft tissues referenced in the previous two issues of JMS (Science of Massage Institute » SCIENCE OF MEDICAL MASSAGE THERAPY. Part I: Introduction to the Reflex Zones Concept AND Science of Massage Institute » SCIENCE OF MEDICAL MASSAGE THERAPY. Part II: Reflex Zones In Somatic Disorders).
We recently published several clinical cases of Medical Massage application for the patients with chronic visceral disorders from our clinic and from clinics associated with the Science Of Massage Institute. Surprisingly, these publications triggered some negative feedback from several therapists and ‘experts’ who proclaimed that Massage Therapy (MT) doesn’t have any therapeutic impact on chronic visceral disorders. Thus, critics denounced an entire branch of modern medicine where Medical Massage Therapy plays an essential role. In a sense, this article responds to these uninformed comments while hoping to extend the professional horizons of clinically oriented therapists.
Medical Massage therapy for patients with chronic visceral disorders relies heavily on its reflex mechanism. Thus, before we review this vital subject, we would like to cite two scientists on this matter Dr. J. Weiss, MD (1952) from the USA and Prof. A.M. Aksenova, MD (1998) from the Russian Federation:
‘Reflex value of massage is probably the most important of all. From this point of view, we may retain conventional estimate of the merits of massage.”
Dr. Weiss (1952)
“The treatment of any chronic disorder of the human body has to include the appropriate method of massage therapy.”
Prof. Aksenova (1998)
BRIEF HISTORY OF MEDICAL MASSAGE ON CHRONIC VISCERAL DISORDERS
The clinical role of Medical Massage in the treatment of chronic visceral disorders consists of two equal components: reflex and local (in the form of abdominal massage) effects of massage therapy. Unfortunately, therapists can use both mechanisms only in the gastrointestinal, and to a lesser degree, for hepatic, urinary, and reproductive disorders. However, in cardiac, pulmonary, or endocrine disorders, the therapist has only one option – the reflex mechanism of MT. The reflex mechanism of MT relies on the presence of the so-called viscera-somatic, and viscera-motor reflexes in the human body. Scientifically speaking, the concept of reflexes was finalized by Prof. Irwin Korr in 1947 and 1949.
The presence and role of viscera-somatic and viscera-motor reflexes were also examined by other scientists and physicians who published maps of their distribution throughout the human body: Chapman Reflexes (Chapman et al., 1932), Glezer/Dalicho Zones (Glezer and Dalicho, 1955), etc. Now practitioners may use these maps as guides to better aim therapy and help patients with chronic visceral disorders.
Before we move forward, we need to discuss one crucial issue. In cases of pure somatic abnormalities, such as Carpal Tunnel Syndrome or Headaches, MM is a decisive therapy that can, in most cases, eliminate the pathology on its own. In cases of chronic visceral disorders, MM plays an important but supportive role. There is no way MM can cure emphysema, for example, but at the same time, it significantly contributes to its medical management by physicians responsible for the entire treatment. MM therapy does this by eliminating reflex zones formed in soft tissues secondarily or by preventing their formation. The use of MM results in less frequent flare-ups, a lesser dosage of medications, and patients’ improved response to medical therapy.
CHRONIC VISCERAL DISORDERS AND REFLEX ZONES FORMATION IN SOFT TISSUES
CNS supports our inner organs, soft tissues, bones, and our entire circulation. The innervation pattern is very segmental and gives the body great flexibility and room for the immediate reactions necessary to adjust to outer or inner bodily changes. The body’s segmental pattern of innervation is a direct result of the spinal cord’s segmental arrangement. In this case, sensory data from the peripheral receptors to the CNS and motor response from the CNS to the organs and tissues have an exact execution level.
For example, the T1 segment of the spinal cord innervates part of the skin (i.e., dermatome), pectoralis, and latissimus dorsi muscles with covering fascia (i.e., myotome), periosteum of the corresponding rib, lower angle of scapula and humerus (i.e., sclerotome), artery and vein (i.e., vasotome), as well as the lungs and heart (i.e., visceratome). Thus, somatic structures (skin, muscles, etc.) share the same source of innervation as inner organs (lungs and heart in the discussed case). This anatomical fact is the foundation for the reflex mechanism of MM in cases of chronic visceral disorders. Let’s look at this important issue in greater detail using pulmonary pathology located in the middle lobe of the right lung as an example.
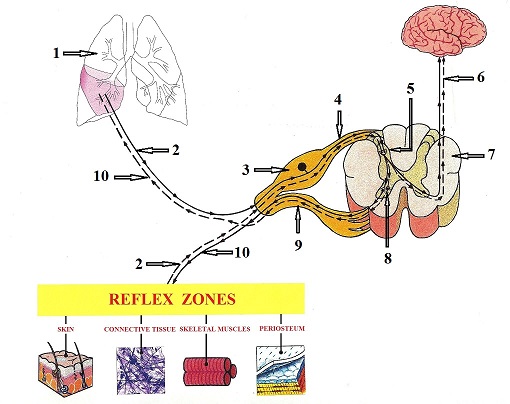
First of all, let us get familiar with major players involved in this process with the help of Fig. 1.
|
1 – right lung with pneumonia |
6 – flow of sensory impulses to the brain |
|
2 – ascending sensory neuron |
7 – segment of the spinal cord (cross-section) |
|
3 – dorsal root ganglion |
8 – anterior horn (motor commands center) |
|
4 – dorsal root |
9 – ventral root |
|
5 – posterior horn (sensory computer) |
10 – descending motor neuron |
Now we will bring the entire process to life with the help of the interactive diagram presented in Fig. 2. It illustrates the mechanism of reflex zones formation in the soft tissues as a reaction to pneumonia.
Fig. 2. Mechanism of reflex zones formation in the soft tissues as a reaction to pneumonia
Since the early stages of the pulmonary disorder, the sensory stimulation evoked by the original pathological process bombards the segments of the spinal cord that are responsible for the innervation of the middle lobe of the right lung. This process is indicated by the FIRST BLUE DOT moving along the ascending nervous pathway from the lungs to the posterior horns of the spinal cord, where this information is initially processed. The posterior horns of the spinal cord work as a sensory computer that analyzes the initial input from the stimulated peripheral receptors and conducts this information to the different parts of the CNS.
From the posterior horns, the sensory stimuli travel in two directions within the CNS. The movement of the FIRST GREEN DOT indicates that the ascending information now continues to move up to the brain creating the unpleasant sensations of chest heaviness, fever, etc. These uncomfortable sensations keep the patient in bed, refrain him or her from exposure to low temperatures, and the patient starts to seek medical help by contacting a family physician or pulmonologist. Thus, the ascending sensory flow from the peripheral receptors in the lungs finally reaches the brain, it changes the patient’s behavior to help the body fight against the infection more efficiently.
The movement of the SECOND GREEN DOT indicates the conductance of the sensory stimuli within the same segment of the spinal cord from the posterior horns of the spinal cord to the anterior horns. The anterior horns of the spinal cord are the lower motor command centers that are responsible for the generation of motor commands back to the stimulated area.
In the case of pneumonia, the sensory stimuli report to the CNS the accumulation of the sputum inside the bronchial tree, narrowing airways, and dropping blood oxygen levels. This sensory information triggers the motor response in the form of cough, labored breathing, etc. These are the body’s primary protective reactions that help with recovery. Therefore, the motor commands from the anterior horns of the spinal cord flow back to the parts of the lungs where the initial sensory stimulation occurred (accumulation of sputum – cough), trying to correct pathological symptoms. This process is indicated by the movement of the FIRST RED DOT back to the lungs along the descending nervous pathways. The lower motor centers in the anterior horns cannot distinguish where they send motor innervation to because of the so-called Phenomenon Of Convergence, which we will discuss later.
As soon as the lower motor centers are activated, they send motor commands to every organ or tissue this segment of the spinal cord innervates. Thus, the motor commands delivered to the lungs also lend to the soft tissues innervated by the same segment of the spinal cord as the affected part of the lung. This process is shown as the SECOND RED DOT that travels from the lower motor centers to the skin, connective tissue structures, skeletal muscles, and periosteum innervated by the same spinal cord segment the affected the lobe of the right lung. At this point, the soft tissues start to receive motor commands, which are entirely unneeded since there was no initial sensory stimulation of the peripheral receptors located in the soft tissues.
After the soft tissues’ repeated bombardment by unnecessary motor commands, various pathological abnormalities such as tingling or burning pain in the skin, fascia shortening, muscle tension or pain and tension in the periosteum, etc., start to develop in the soft tissues that share the same innervation with the affected parts of the lungs. These soft-tissue abnormalities are the pure reflex reactions of the soft tissues to the presence of visceral pathology (inflammation in the middle lobe of the right lung in the discussed case). They are called reflex zones.
As soon as reflex zones form in the soft tissue, the peripheral receptors located there begin to emit their sensory stimuli to the same segment of the spinal cord (shown as the SECOND BLUE DOT in Fig. 2), which travel from the reflex zone areas to the spinal cord. As soon as the same sensory computer in the posterior horns is activated by information from the soft tissues, it starts to send signals to the brain (THIRD GREEN DOT), and the patient begins to feel the sensation of tension in the soft tissues, burning sensation in the skin, restriction of at the end of ROM, etc. Simultaneously, the sensory stimuli travel to the lower motor centers in the anterior horns (the FOURTH GREEN DOT travels to the anterior horns).
As soon as the lower motor centers are activated, they send the motor signals back to the soft tissue in the reflex zone areas (THIRD RED DOT). Simultaneously, these now unnecessary motor commands arrive at the affected areas of the lungs (FOURTH RED DOT), and they additionally irritate the inflamed areas. Thus, reflex zones in the soft tissue become an additional factor that exacerbates the original clinical picture of pneumonia.
The somatic practitioner’s job is to detect and eliminate reflex zones in the soft tissues that have formed secondarily to the original pathological process in the inner organ, and Medical Massage therapy is the best tool for the job. The practitioner plays a vital role in the integrative approach to rehabilitating patients with various visceral disorders, including chronic pneumonia. We completely agree with Dr. Nansel and Dr. Szlazak (1995), who wrote:
“Nociceptive input from dysfunctional somatic structures may act to exacerbate the symptoms of pre-existing visceral disease. This very well provides ample justification for the role of the somatic therapist in the co-management of the patient’s overall symptoms.”
Clearly, it is the practitioner’s job to prevent the formation of reflex zones using therapeutic massage or to eliminate them using Medical Massage therapy specifically designed to treat chronic visceral abnormalities.
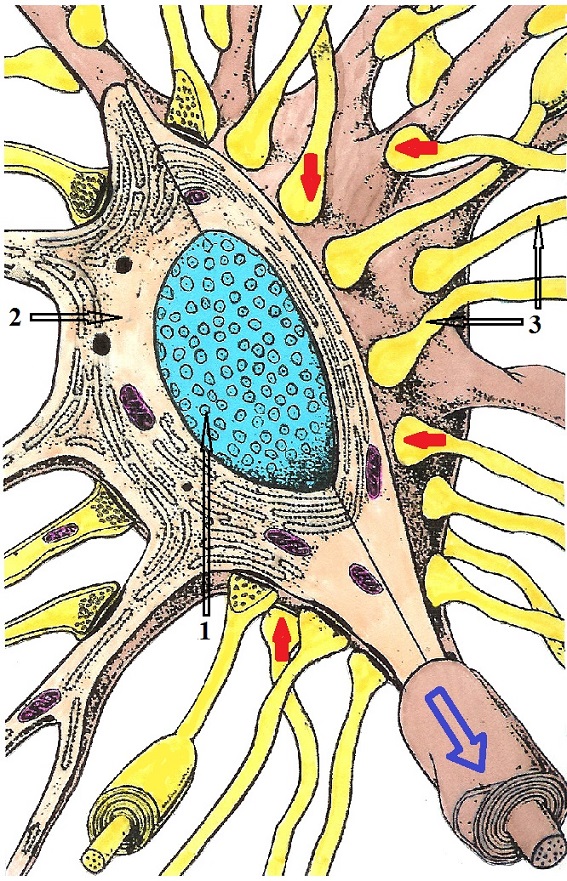
PHENOMENON OF CONVERGENCE
The final subject of this article is the Phenomenon of Convergence: Why are chronic visceral abnormalities responsible for forming reflex zones contribute to the further progression of the original pathological process in the affected inner organ? Please look at Fig. 3 which shows the structure of the spinal neuron located in the posterior horns of the spinal cord. What you see is a picture of one of the sensory computers we discussed above.
1 – nucleus of the spinal neuron
2 – cytoplasm of the spinal neuron
3 – ascending sensory pathways from various somatic and visceral structures land on the body of the spinal neuron
Red arrows – sensory information arrives from peripheral receptors.
Blue arrow – spinal neuron conducts processed sensory information into the CNS.
Because posterior horns are a relatively small part of the spinal cord it’s simply impossible for each spinal neuron to contact only with one group of the peripheral receptors. Simply put, there is no room to do that. Therefore, several ascending sensory pathways that deliver information from the peripheral receptors to the spinal cord land on the body of the same spinal neuron.
Suppose we continue to use our patient with right-side, middle-lobar pneumonia as an example. In this case, we may see those sensory fibers from different organs and tissues land on the body of the same spinal neuron. The spinal neuron will be equally stimulated by impulses from the lungs and from, let us say, the right latissimus dorsi muscle which reports to the same segment of the spinal cord. Each of these stimulations will, to an equal degree, activate the lower motor neurons. Their activation will send motor commands to all tissues and inner organs innervated by the same spinal cord segment, forming a vicious cycle of codependent pathologies. The longer the symptoms of pneumonia are present, the more reflex zones develop in the soft tissue, which exacerbates the maintenance of pulmonary inflammation. To quote one of the most prestigious American medical publications on the subject of rehabilitation Physical Medicine and Rehabilitation (1996):
“All somatic and visceral tissues can be negatively affected if they are innervated by the nerves from a spinal segment that receives afferent information from an area of dysfunction. If this is true, then it follows that alleviation of somatic dysfunction via massage can result in optimized function of somatic and visceral systems that are innervated by the same spinal segment.”
Professor J.W. Atchison, Dr. S.T. Stoll, Dr. G. Gilliard
CONCLUSION
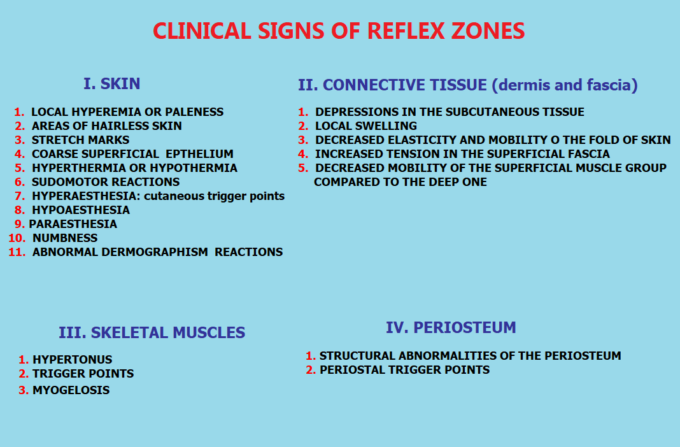
The physician responsible for the patient’s therapy must be fully informed of the therapist’s treatment plan and permit to proceed. To treat patients with chronic visceral disorders, the therapist must be trained in understanding and adequately testing each type of soft tissue (skin, fascia, muscles, periosteum) for possible signs of reflex zone formations. When these reflex changes are detected, they must be eliminated using proper MM techniques and modalities. Fig. 4 summarizes the list of reflex changes in each layer of soft tissues which must be examined and detected by the therapist.
Finally, we would like to address the issue of Abdominal Massage (AM). Yes, AM is an essential part of therapy for patients with various chronic abnormalities in the function of the abdominal and pelvic organs. Recently, publications on this subject started to appear amidst professional US massage sources. Unfortunately, these publications exhibited incorrect and harmful recommendations.
The practice of AM requires a deep understanding of the nature of various abdominal and pelvic pathologies, their reflex interactions, and extensive training in technique application with an experienced instructor. There is no room for educators’ or therapist’s personal opinions in this part of the profession because incorrect AM in the abdominal and pelvic regions will significantly worsen the patient’s condition and trigger clinical flare-ups. We want to warn therapists of sources that spread misleading and dangerous information.
From our analysis of the field, we suggest Dr. Jean-Pierre Barral, DO as only a reliable scientifically and clinically grounded source for AM training. SOMI will also offer training in AM to our former students who already practice Medical Massage successfully and are now considering expanding their practice to the domain of visceral pathologies.
REFERENCES
Aksenova, A.M., Romanova M.M. Influence of Reflex Massage of Skeletal Muscles on Metabolism of Patients With Complicated Gastric Ulcers. Vopr. Kurorto. Fizioter Lech Fiz Kult, 6:24-26, 1, 1998
Atchison J.W, Stoll S.T., Gilliard G. Physical Medicine and Rehabilitation. Elsevier Sunders, Philadelphia, 1996
Chapman, F., Chapman, A.H., Owens, G. Chapman’s Reflexes. Rowan Printing Company, Salisbury, NC, 1932.
Glezer O., Dalicho V.A. Segmentmassage. Leipzig, 1955
Korr, I.M. The Neural Basis of the Osteopathic Lesion. JAOA, 47(4): 191-198, 1947.
Korr, I.M. Skin Resistance Patterns Associated With Visceral Disease. Fed. Proc., 8:87-88, 1949.
Nansel D., Szlazak M. Somatic Dysfunction and the Phenomenon of Visceral Disease Simulation: A Probable Explanation for the Apparent Effectiveness of Somatic Therapy in Patients to be Suffering from True Visceral Diseases JMPT. 18(6) 379-384,1995
Washington K, Mosiello R, Venditto M, Simelaro J, Coughlin P, Crow WT, Nicholas A. Presence of Chapman reflex points in hospitalized patients with pneumonia. JAOA, Oct. 2003
Weiss J.M. In: Ebel A., Wisham L.H. Effect of Massage On Muscle Temperature and Radiosodium Clearance. Arch Phys Med, July:399-405, 1952
Category: Medical Massage
Tags: 2021 Issue #1